By: Dr. Elizabeth Eggert
Did you know that stress can affect your oral health?
Stress is, unfortunately, part of all of our lives. And while most people are aware of the effect stress can have on their physical health, often the link between stress and oral health isn’t as clear.
And yet stress can have a significant impact on your oral health. The effects of chronic stress can show up in your mouth, teeth, gums, and jaws as gum disease, teeth grinding, jaw clenching, and more. Understanding how stress can affect your oral health is essential to maintaining a healthy smile.
Here, we’ll explore the effects of stress on oral health along with some practical strategies to manage stress and support your smile.
Stress and Oral Health: Unraveling the Connection
Learning to recognize the conditions caused or worsened by stress is vital to timely intervention. Chronic stress can lead to a number of oral health problems, including:
Bruxism: The Grind Behind Stress

Stress can cause tension in your jaw, which can lead to bruxism. Bruxism is a condition where you unconsciously grind or clench your teeth. Many people with this problem are unaware of it as it happens most often while they are sleeping, however, it can even happen during the day without conscious awareness of it.
Because the force exerted while clenching or grinding is often much more than that exerted while chewing, it can result in significantly worn-down teeth, jaw pain, headaches, damage to dental restorations, and in many cases, even fractures.
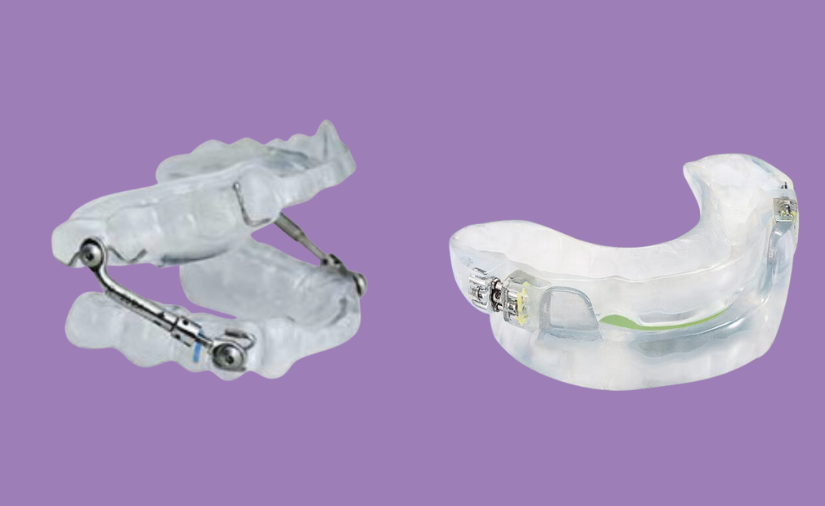
If you think you may be grinding or clenching your teeth, talk with Dr. Elizabeth Eggert or Dr. Jeff Eggert in North Oaks, MN about obtaining a custom-fitted night guard to help protect your teeth from stress-related wear and tear.
Gum Disease: Stressing Out Your Gums
Stress can weaken your immune system, making you more susceptible to infections and your gums more susceptible to inflammation and gum disease. Gum inflammation, bleeding, tenderness, and periodontal disease are more likely when you are under chronic stress.
If you notice your gums are red or swollen or that they bleed when you brush or floss, make an appointment with Dr. Elizabeth Eggert or Dr. Jeff Eggert right away as bleeding in the gums is a sure sign of unwanted inflammation
Temporomandibular Joint Disorders (TMJ): Stressing Over Your Jaw
TMD (or more commonly called “TMJ”) is a disorder affecting the jaw joint, causing symptoms like jaw pain, stiffness, clicking or popping, and difficulty opening or closing the mouth. Chronic stress can cause you to clench your teeth and jaw, which can stress the temporomandibular joints, leading to TMD. Lack of sleep due to stress can further exacerbate this issue.
If you notice any signs of TMD, speak with Dr. Elizabeth Eggert or Dr. Jeff Eggert at Eggert Family Dentistry. Similar to bruxism, we may recommend an appliance to ease your jaw discomfort and protect your joints from wear.
Canker Sores: Stress Taking Its Toll Inside Your Mouth

Stress can also bring on canker sores inside your mouth, which can cause pain and discomfort. Canker sores are small round ulcers in your mouth, often found on the inside of your cheeks and lips or on your tongue and gums.
While these sores typically go away on their own, it’s helpful to understand what causes them and how to mitigate your discomfort while they heal. While the specific cause of canker sores is still unknown, there does seem to be a strong link between canker sores and stress.
If you experience canker sores, you can help manage your discomfort by:
- Swishing a warm salt water solution around your mouth multiple times per day (8 oz warm water and 1 tsp salt)
- Drinking cold liquids through a straw
- Eating soft foods
- Avoiding sugary, salty, spicy, acidic, or very hot foods
- Using a soft-bristled toothbrush when brushing your teeth
When you are under significant stress, it can be tempting to neglect your regular oral hygiene routine. But maintaining routine brushing, flossing, and dental visits with Dr. Elizabeth Eggert or Dr. Jeff Eggert is vital to maintain the health of your teeth and gums.
Managing Stress to Preserve Oral Health
In addition to maintaining a consistent oral health regimen, implementing some or all of the following healthy habits can help improve your body’s resilience to stress and support your oral health.

Stay Hydrated
Drink plenty of water. Maintaining adequate hydration helps support saliva production and overall oral health.
Eat a Healthy Diet
Include a wide variety of fruits, vegetables, lean proteins, and whole grains in your daily diet. Limit sugary treats, caffeine, and alcohol — too much of these can exacerbate stress and negatively impact your oral health.
Get Regular Exercise
When you exercise, your body releases endorphins, a natural stress reliever. Being active also helps promote better sleep, which aids in stress management and benefits your physical and dental health.
Prioritize Quality Sleep
Stick to a regular sleeping schedule to ensure adequate sleep. Establish a bedtime routine that helps you relax and ease tension in your jaw. This could include a jaw massage, gentle stretching, deep breathing techniques, or aromatherapy.
Implement Stress-Relief Techniques
Stress-relief techniques like deep breathing, mindfulness meditation, a warm bath, and yoga can help you unwind, relax your jaw, and lower overall stress levels. Experiment with a variety of stress-relief techniques to find the ones that work best for you.
Ask for Help
If stress feels overwhelming or becomes chronic, consider seeking professional support from a therapist or counselor who specializes in stress and anxiety management. Having someone to talk through stressful feelings with can be immensely beneficial to your mental and physical health (including your oral health!).
Stress and oral health are inextricably linked. Taking the time and energy to invest in your physical, mental, and emotional well-being leads to improved health and happiness, and a reduced likelihood of developing stress-related oral health issues.
At Eggert Family Dentistry, we know your mental health affects your oral health and we believe they are equally important components of overall wellness. If you’re concerned your oral health is being compromised by stress or anxiety, we recommend making an appointment with your primary physician as well as with Dr. Elizabeth Eggert or Dr. Jeff Eggert at 651.482.8412. We’re always here to help!










 When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others:
When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others: Did you know that, in
Did you know that, in  Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.