By: Dr. Elizabeth Eggert
In many ways, the stage for lifelong health is set in childhood. Often overlooked amid the busyness of parenting, mouth-breathing can affect your child’s airway and oral health and affect their quality of life. As a parent, you are your child’s biggest advocate. That’s why we want to take some time to educate you on the topic of airway and oral health, including signs to watch for and what you can do if you suspect your child’s airway is compromised.
Contributing factors that affect airway and oral health
While it may be necessary during allergy season or when fighting a head cold, long-term mouth-breathing will result in airway issues or sleep-disordered breathing.
Certain malformations such as crooked, misaligned teeth, improper jaw alignment, a narrow palate, and abnormalities of the head or skull can also make nasal breathing difficult. Children who deal with these challenges often unknowingly default to mouth-breathing. Interestingly, sometimes it’s a matter of what comes first – the chicken or the egg, because in children who mouth breathe, their development will occur in a more vertical pattern, resulting in the malformations noted above. This also makes things more difficult the longer we wait for intervention.
When your child breathes through their nose, their body filters toxins and debris through the nose’s cilia. Nasal breathing also helps the body produce nitric oxide, which makes it easier for the lungs to absorb oxygen. Plus, nasal breathing warms and humidifies the air in the nasal cavity, keeping the tonsils and adenoids moist and healthy.
Mouth-breathing, on the other hand, dries out tonsils and adenoids, making them irritated and inflamed and exacerbating breathing issues. A dry airway is also more prone to collapsing, and will cause childhood sleep apnea.
Additionally, mouth-breathing deprives your child of oxygen by up to 20% and increases CO2 levels in their blood.
Over time, stressors resulting from mouth-breathing can even lead to hypertension, heart disease, diabetes, lung malfunction, and enlargement of the right ventricle of the heart.
How do I know if my child is a mouth-breather or dealing with an airway obstruction?
When a child is mouth-breathing, their mouth is drier and doesn’t have adequate saliva to protect their teeth and gums against damaging bacteria. The increased presence of bacteria often results in more plaque, tooth decay, and gum disease. Generally, if the lips are apart, breathing is occurring through the mouth instead of through the nose.
- Some additional signs that your child may be mouth-breathing as opposed to nasal breathing include:Snoring
- Poor speech
- Halitosis
- Dry lips
- Bedwetting
- Fatigue/dark circles under the eyes
- Insomnia
- Brain fog
- Academic struggles
- ADHD symptoms
- Forward head posture (bent neck)
- Sleeping with their neck extended
The role of healthy childhood habits on airway and oral health
Fortunately, as a parent, you’re not a helpless bystander when it comes to detecting airway issues in your child…or when it comes to helping prevent them. There are many healthy habits you can help your child develop that will decrease their risk.
If you notice your child mouth-breathing, encourage them to breathe through their nose instead. Sometimes, children continue to mouth-breathe long after a cold or allergies have subsided. Consider teaching your child relaxing nasal breathing techniques they can practice during the day and while they’re falling asleep at night. Always think “tongue up, lips sealed, breath goes in through the nose.”
Encourage your child to eat healthy and stay hydrated. Healthy food is an important part of keeping your child’s immune system strong. Proper hydration ensures adequate saliva production, which keeps your child’s oral biome healthy.
Make sure your child gets plenty of sleep. Just like healthy food, good sleep helps strengthen weak immune systems and keeps healthy immune systems strong!
Make sure your child stays active. Physical activity strengthens the respiratory system.
Encourage your child to brush and floss their teeth every day. It reduces the buildup of bacteria in your child’s mouth that could irritate their airways.
The importance of regular recare visits
Last but certainly not least, perhaps the most important thing you can do to help your child prevent airway issues and ensuing long-term health issues is to schedule regular recare visits at Eggert Family Dentistry! We recommend starting your child’s recare visits before their first birthday! Our recare visits are thorough! We go above and beyond simply looking for cavities and cleaning your child’s teeth. In addition to cavities, we look for various dental problems that can be linked to airway issues or sleep-disordered breathing. These dental problems include:
- Bruxism
- Functional tooth wear and fractures
- Erosive tooth wear
- TMD/myofascial pain
- Malocclusion, especially anterior open bite and crossbite
- Facial development
- Periodontal disease
- Abfractions
- Impacted teeth
- Orthodontic or orthognathic relapse
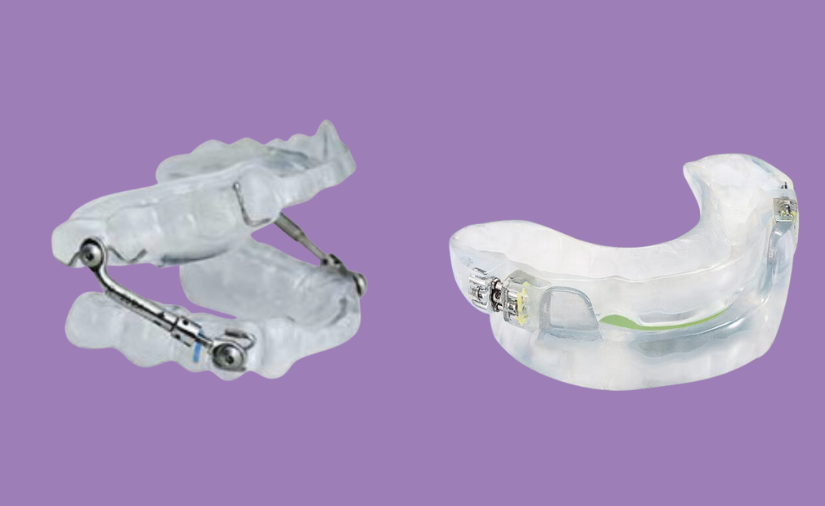
If Dr. Elizabeth Eggert or Dr. Jeff Eggert is suspicious your child is struggling with airway issues or sleep-disordered breathing, they may suggest a myobrace appliance, which is kind of like a mouthguard, to correct their bite and facilitate nasal breathing. In some cases, they will refer your child to an ENT.
Being proactive is key. When you partner with Dr. Elizabeth Eggert or Dr. Jeff Eggert for your child’s dental care, they help your child grow up healthier and have an optimal quality of life. At Eggert Family Dentistry, we recognize that airway and oral health are critical for lifelong physical health and self-esteem and set your child up for academic and athletic success throughout childhood, adolescence, and adulthood. Call us today at 651.482.8412 to set up your child’s next recare visit in our office!
Want to learn more?
If you’re interested in the connection between dental problems and airway issues, we highly recommend these books:
- Sleep Interrupted by Steven Park, MD
- The Chronic Cough Enigma by Dr. Jamie Koufman
- No More Allergies, Asthma or Sinus Infections by Dr. Lori Jones
- Close Your Mouth by Patrick McKeown
- The Oxygen Advantage by Patrick McKeown