By: Dr. Elizabeth Eggert
How did this start?
Molly came to us with questions during her recare appointment. She had recently had a sleep study done with her doctor and had been diagnosed with Mild Sleep Apnea. She was given a CPAP (Continuous Positive Airway Pressure) machine to try, but wanted to know her other options as the CPAP wasn’t working out that well for her. CPAP therapy is the “gold standard” treatment for sleep apnea, but due to the high air pressure needed to prevent the collapse of the airway, some patients find that they just can’t tolerate the therapy. Molly knew about the Seattle Protocol from our blog articles and wanted to know more.
Molly suffered from acid reflux and had severe demineralization and decay with her teeth. She told us she never really slept well and had been taking Ambien for 15 years to help with her sleep issues. Despite the medication, she still found that most afternoons or evenings she needed a nap to help combat her excessive fatigue.
What did Molly want?
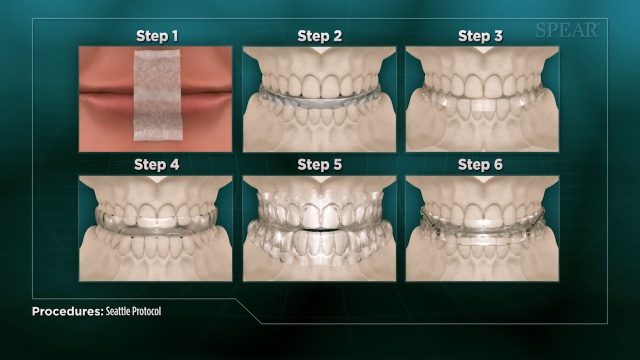
Molly wanted to sleep better. She didn’t want to be so fatigued. And, she wanted something more comfortable than the CPAP option for her sleep issues. We talked to Molly about the possibility to undergo the Seattle Protocol to see if using a nighttime appliance could help her sleep better. The Seattle Protocol is a six-step process that runs patients through different types of appliance options to see what is the most non-invasive appliance/splint to improve sleep. Typically at one of the six stages, patients will feel better and the symptoms they have from sleep-disordered breathing or sleep apnea will improve significantly. With the Seattle Protocol, each step builds upon the last, but patients don’t necessarily need to complete the entire process as the purpose of the protocol is to determine the phase that provides the best relief of symptoms.
What was involved?
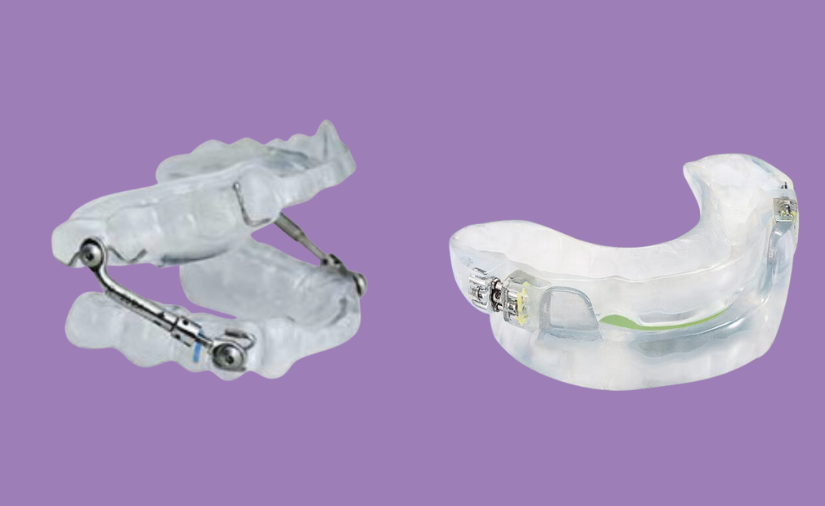
We did a comprehensive evaluation of Molly’s bite and function to be sure that having her wear a nighttime appliance wouldn’t trigger any joint, muscle, or teeth issues for her. Then, we started Molly with the first phase of the Protocol – Nose Clearing and Mouth Taping. The purpose of mouth taping is to keep your body breathing through your nose, which is the most healthy way to breathe. Mouth taping should only be done under a doctor or dentist supervision, however. Molly did well with the mouth taping and then we worked her through the Protocol using the myTap appliance. The different stages of the Protocol involve different parts of myTap.

Moving through the stages of the Protocol, Molly reported that she was sleeping better and napping less. She found the Stage 3 version of the myTap appliance to be the most effective for her. In this stage, the patient wears a lower arch appliance that holds them in a more forward position.
Molly tried stages 4 and 5 as well, but really felt the most comfortable and the most rested in the Stage 3 appliance so we took impressions of her mouth and had a Mandibular Pull Forward appliance fabricated to custom fit her mouth.

What does Molly think now?
Molly loves her nighttime appliance. She has been wearing it nearly 3 years now and doesn’t want to go back! She reports, “It has just made such a huge difference in being able to function in everyday life. I used to have to take an hour nap every day, but don’t have to anymore.” Molly has had no issues with her teeth or bite changing, as this can be a real side-effect of traditional sleep apnea appliances. She finds her appliance very comfortable.
Molly notes that it might be easy to perceive the Seattle Protocol as being a “great inconvenience,” but she wants to assure people that “IT JUST IS NOT!” Getting used to mouth taping and having an appliance in her mouth were something new, but Molly is so glad she did it because “I couldn’t tolerate the CPAP and my appliance is just SO much better!”
She was very happy to work with Dr. Elizabeth Eggert and liked the attention she paid to having a shared goal. If you have sleep issues, Molly would recommend you have a conversation with the team at Eggert Family Dentistry.
“The entire team is amazing!”












 The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck.
The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck. A
A