By: Dr. Elizabeth Eggert
Chronic or intense jaw pain can be debilitating, making it difficult to speak or eat properly. When the pain is severe enough, it can even disrupt your sleep or limit your ability to function normally in your everyday life.
Jaw pain can include jaw tenderness, pain when you bite down, pain in or around your ears, and headaches. There are many possible causes of jaw pain, so it can be challenging to diagnose what is causing it.
Read on to learn some of the common causes of acute jaw pain and how we treat it here at Eggert Family Dentistry using a device called the Aqualizer®.
Common Causes of Jaw Pain
While over-the-counter painkillers and anti-inflammatories can temporarily reduce jaw pain, to properly treat it you need to determine the root cause.
There are several conditions that can contribute to severe jaw pain, some of which are related to dental health, but not all. It’s important to consult both Dr. Eggert and your physician to diagnose the cause of your jaw pain. They will do a thorough exam, which may include dental X-rays, CT scans, or blood work.
The most common causes of jaw pain include:
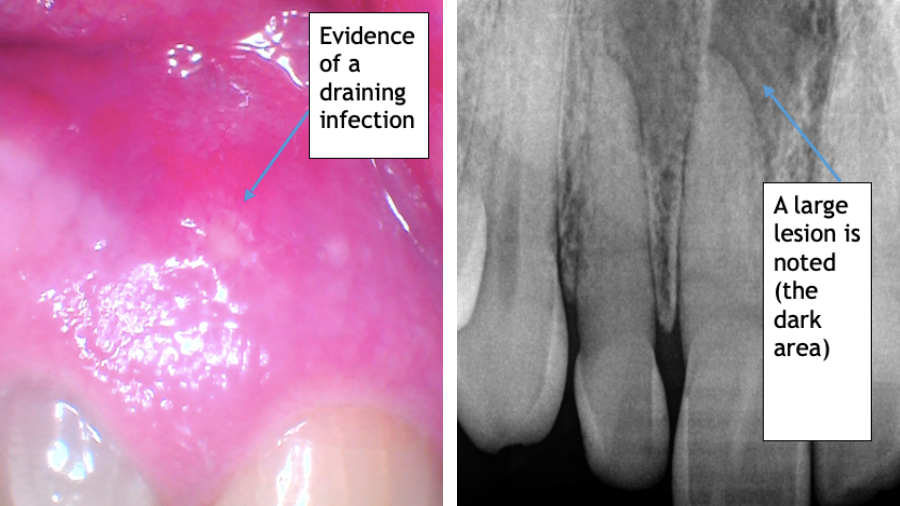
Decayed or Abscessed Teeth
Pain from tooth decay or a tooth abscess can radiate to the jaw. Treatment may include fillings, crowns, a root canal, or extraction, depending on the severity of the problem.
Gum Infection
A gum infection is usually caused by bacteria that multiplies due to poor oral hygiene. The most effective initial treatment is a deep cleaning called scaling and root planing. Occasionally adding localized antibiotics can also improve the infection. Improved oral hygiene can help manage the gum disease caused by a gum infection and hopefully prevent future acute incidents.
Cluster Headaches or Migraines
A migraine typically presents as a throbbing headache on one side of the head, while a cluster headache usually starts as pain behind or around one of the eyes. Both can also send pain to the jaw. There are also times when overuse of the jaw muscles or jaw joint can send pain signals that manifest as cluster headaches or migraines.
Sinus or Ear Infections
Infections of the sinuses or ear canals can also cause pain to radiate to the jaw. When sinuses or ears become infected, often an excess of mucus puts pressure on the jaw joint, causing pain.
Heart Attack or Angina
Jaw pain can sometimes accompany a heart attack or angina. During a heart attack, pain can radiate to the arms, back, neck, or jaw. Women are especially likely to experience jaw pain on the left side when having a heart attack.
If you experience any of the following symptoms along with your jaw pain (even if you don’t have chest pain) you should immediately call 911:
- Chest discomfort
- Shortness of breath
- Sweating
- Nausea
- Feeling faint
Trigeminal Neuralgia
Trigeminal neuralgia is a condition commonly caused by compression of the trigeminal nerve—a large, three-part cranial nerve that provides sensation to a large portion of the face, including the upper and lower jaws. This condition causes brief but excruciating jaw and facial pain on one side of the face. It can feel like shooting, stabbing, or electrical pain, and can mimic dental pain. Treatment for trigeminal neuralgia typically involves medication or surgery.
TMJ or TMD
Temporomandibular joint (TMJ) dysfunction, or Temporomandibular Disorder (TMD) are the most common causes of jaw pain. The temporomandibular joints are the hinge joints on each side of your jaw. Pain can originate in either the joints themselves or the muscles surrounding the joints. This condition can be difficult to treat because there are multiple potential causes, including: muscle pain, jaw joint injury, overstimulation of the jaw joint, a displaced disc, or arthritis of the protective disc that cushions the jaw joint.
Damage to the jaw joint or the muscles that control your jaw movement can be caused by several factors, including:
- Grinding your teeth
- Involuntarily clenching your jaw due to stress or anxiety
- Jaw joint trauma, such as a sports injury or other facial injury
- Upper airway resistance syndrome (UARS) and lack of reparative sleep
TMJ or TMD muscle tension can often be treated with muscle relaxants, anti-inflammatory drugs, or a custom fitted dental orthotic (similar in concept and shape to a mouth guard). Joint dysfunction is generally treated with anti-inflammatories and sometimes arthroscopic surgery.
Bruxism
A person with Bruxism grinds or clenches their teeth, either while sleeping or even throughout the day—and in most cases, they don’t realize they’re doing it. Bruxism is generally caused by stress, and it can, in turn, cause jaw pain. Bruxism can often be treated using a custom fitted dental orthotic—a splint typically worn at night, but sometimes with some day use if needed.
Treating Acute Jaw Pain with the Aqualizer®
At Eggert Family Dentistry, Dr. Elizabeth and Dr. Jeff use a device called the Aqualizer® to treat acute jaw pain.
The Aqualizer® is a self-adjusting dental splint used to diagnose how much a patient’s dental bite contributes to their jaw or facial pain. The extent that it helps relieve this pain indicates whether dental treatment will be an effective solution.
The Aqualizer® works by allowing the jaw muscles to automatically reposition the jaw to where it naturally works best. It allows the body to correct bite distortions to restore optimal function and balance. Biting down on the Aqualizer® causes the fluid contained in the device to distribute the bite force evenly across the bite, relieving jaw pressure and pain.
This device is meant to be used short-term and is helpful for acute jaw pain related to TMJ or Bruxism. In addition to treating jaw pain, it can also bring relief to chronic neck, shoulder, and migraine pain. It can be very helpful in narrowing in on a diagnosis for your problem.
Are You Suffering with Acute Jaw Pain? Schedule a Visit Today
If you are experiencing jaw pain, Dr. Elizabeth and Dr. Jeff are here to help. Schedule an exam today to determine the cause of your jaw pain and to discuss your treatment options, including whether an Aqualizer® may be right for you. To schedule an appointment, call our office at 651-482-8412.




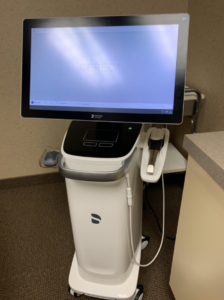 We are happy to now be using the latest scanning unit for our CEREC crowns. The CEREC Prime Scan is a recently developed scanning unit that captures highly detailed images of your mouth.
We are happy to now be using the latest scanning unit for our CEREC crowns. The CEREC Prime Scan is a recently developed scanning unit that captures highly detailed images of your mouth.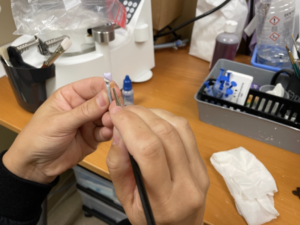 After taking a scan of your teeth, we’re able to create a crown restoration in minutes. New crowns can be made of compressed porcelain, emax porcelain, or compressed composite resin. During your appointment, you can talk with Dr. Elizbeth and Dr. Jeff to determine what material is the best fit for you.
After taking a scan of your teeth, we’re able to create a crown restoration in minutes. New crowns can be made of compressed porcelain, emax porcelain, or compressed composite resin. During your appointment, you can talk with Dr. Elizbeth and Dr. Jeff to determine what material is the best fit for you.