By: Dr. Elizabeth Eggert
School Has Started – and so Have Fall Sports
It seems like summer just started, but alas, school time is here and so are the fall sports that go along with the season change. We want to make sure you included a sports mouthguard in your “back to school” shopping when getting what you need for your athlete.
What Is a Sports Mouthguard?
A sports mouthguard is a piece of clear (or sometimes very colorful) plastic that’s typically worn over the top row of teeth during sports. A mouthguard may also be worn on the bottom teeth, which can be very helpful for people who wear braces or have fixed dental appliances like expanders.
Mouthguards are considered essential equipment for sports that involve body contact or flying equipment, like football, hockey, soccer, volleyball, basketball, wrestling, baseball, lacrosse, and even tennis. However, sports mouthguards can also be beneficial for skateboarding, mountain biking, or other sports where falls could result in mouth injuries. Mouth guards can also prevent dental injuries for people who grind their teeth during sports.
Benefits of a Sports Mouthguard
The biggest benefit of sports mouthguards is that they can prevent a variety of dental injuries and trauma, including:
- Soft tissue damage, such as biting the tongue, cheeks, or lips
- Tooth fractures, including root fractures, broken teeth, or chipped teeth
- Knocked out teeth
- Tooth displacement
- Jaw fractures
- In addition, although medical research is inconclusive, some evidence suggests that sports mouthguards may absorb enough impact between the upper and lower jaws to help reduce concussions.
Mouthguards can also help people save money by preventing the costly need for dental repairs.
Types of Sports Mouthguards
When you are choosing a sports mouthguard, there are three main options to choose from:
- Stock mouthguards: Stock mouthguards are the cheapest and most easily available mouthguard options. Although they come in different sizes, they often don’t fit well. And, a mouthguard that’s too loose or too small can do more damage to your teeth and gums. Finally, these inexpensive mouthguards tend to be made from cheaper materials, making them prone to breaks and tears.
- Boil-and-bite mouthguards: Boil-and-bite mouthguards are also relatively inexpensive and are easily available. Because the mouthguard is boiled to soften the plastic so it can be formed to better fit an athlete’s teeth, the fit is better than what a stock sports mouthguard provides.
- Custom mouthguards: Custom mouthguards are the safest, yet most costly, option available. Dr. Jeff Eggert or Dr. Elizabeth Eggert use impressions of your teeth and mouth to create a mouthguard that fits your teeth perfectly. A custom mouthguard is also the only way to create a precise fit around bridges, braces, and other dental restorations.
Contact Eggert Family Dentistry to Get Fitted for a Custom Sports Mouthguard
When you’re trying to determine which costs to prioritize, remember this: custom sports mouthguards may be more of an investment than the options available online or at retail stores, but they also provide a better fit and are made from stronger material. Finally, investing in a sports mouthguard is considerably less expensive than paying for emergency dental treatment after a preventable injury. Unfortunately, once an injury occurs, it becomes a life-long journey to address the tooth/teeth/or bones involved. In this case prevention is definitely key!

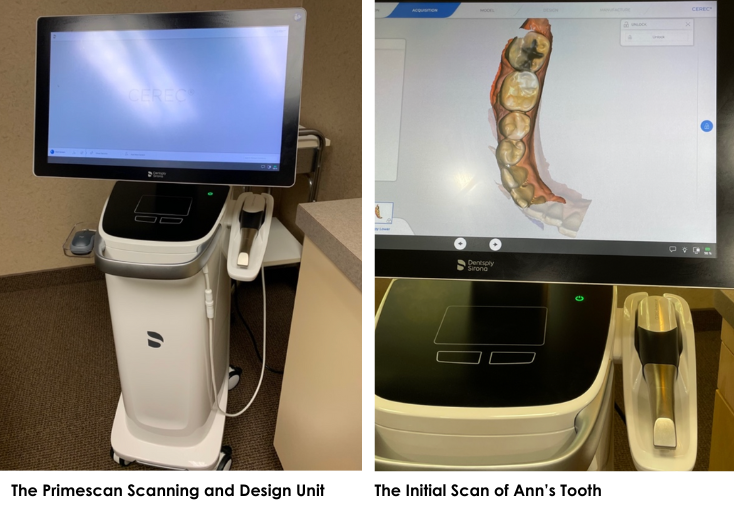
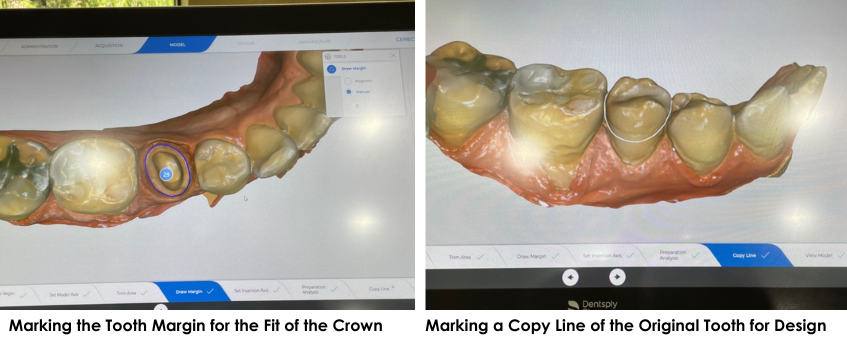
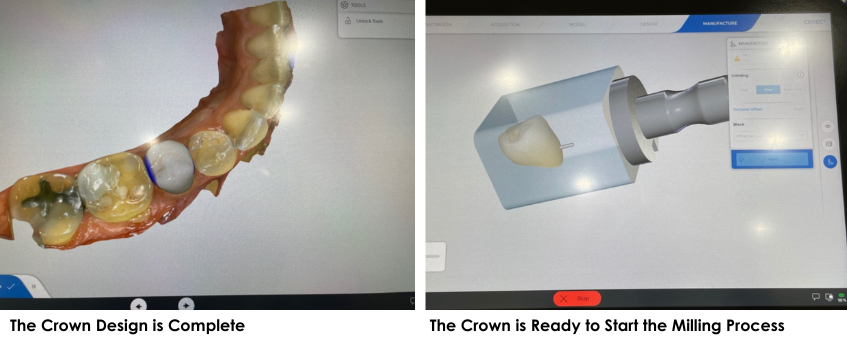

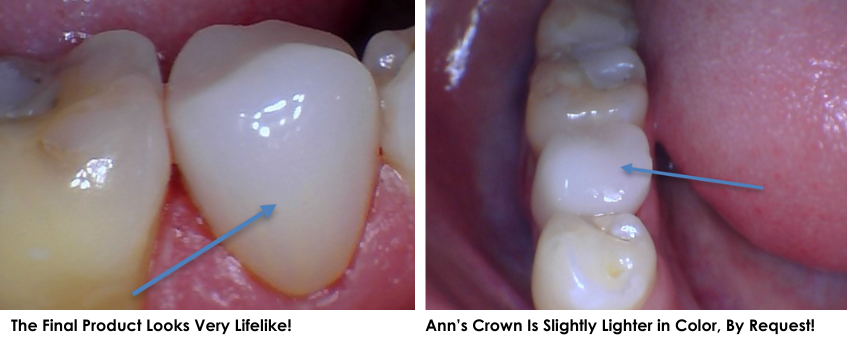



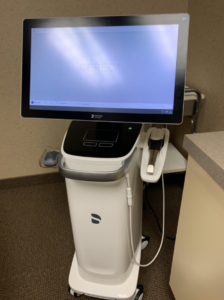 We are happy to now be using the latest scanning unit for our CEREC crowns. The CEREC Prime Scan is a recently developed scanning unit that captures highly detailed images of your mouth.
We are happy to now be using the latest scanning unit for our CEREC crowns. The CEREC Prime Scan is a recently developed scanning unit that captures highly detailed images of your mouth.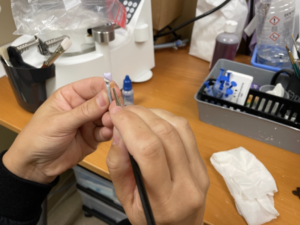 After taking a scan of your teeth, we’re able to create a crown restoration in minutes. New crowns can be made of compressed porcelain, emax porcelain, or compressed composite resin. During your appointment, you can talk with Dr. Elizbeth and Dr. Jeff to determine what material is the best fit for you.
After taking a scan of your teeth, we’re able to create a crown restoration in minutes. New crowns can be made of compressed porcelain, emax porcelain, or compressed composite resin. During your appointment, you can talk with Dr. Elizbeth and Dr. Jeff to determine what material is the best fit for you.