By: Dr. Elizabeth Eggert
We all have different ways and different places we hold stress in the body. Some of us have a tense neck or tight shoulders or a tender lower back, which can all be stress responses to the ups and downs of this complicated world we live in.
From a dental perspective, there’s one stress response we frequently notice in some patients’ mouths: bruxism.
Bruxism is just a fancy word with Greek origins that means grinding the teeth. (It’s also a pretty good Scrabble word to keep in your back pocket, if you’re into that kind of thing.)
People with bruxism may grind or clench their teeth during waking hours without really noticing it, or they may grind or clench their teeth while they sleep. Either way, many or most bruxers aren’t aware that they grind or clench unless someone else alerts them to the situation, such as a dental professional or a sleeping partner. In fact, some bruxers don’t inflict serious damage on their teeth, and discover their bruxism habit due to TMJ problems, chronic headaches, or by recognizing how tense their jaw muscles tend to be.
However, bruxism can have very negative consequences on dental and oral health. Over time, people with bruxism can wear their teeth down to flattened surfaces with an even, square appearance. They may even end up with chipped, loose or even fractured teeth. What’s more, grinding and clenching can damage dental restorations such as crowns or fillings and cause premature failure.
Treating Bruxism with a Dental Splint
There are a variety of ways to treat bruxism.
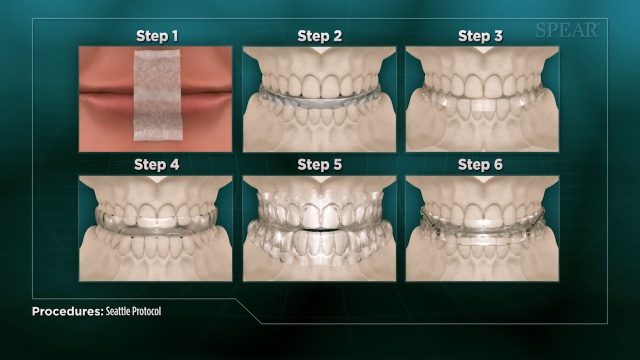
The simplest treatment protects your teeth instantly: An occlusal appliance. This is a custom dental splint designed to be worn while sleeping. It prevents your teeth from touching and it also absorbs bite force. These are different from mouth guards, which are designed to protect your teeth from high-speed foreign objects like baseballs, hockey pucks, or impact with the ground.
Dental splints get high scores in protecting your teeth, but depending on how they are designed, they don’t always discourage the urge to grind, so patients may still suffer from other effects of grinding such as headaches, TMJ issues, and poor jaw mobility.
Other Treatments for Bruxism
There are other potential treatments for bruxism that aim to stop or discourage the grinding behavior, which will help alleviate those non-dental consequences listed above.
These treatments include:
- Treatment for airway issues that may be causing the grinding
- Prescription medications
- Botulinum neurotoxin type A, more commonly known by the brand name Botox
Counter stimulation, such a small electrical impulse that’s activated by clenching - Treating the underlying stress or anxiety that may be causing the bruxism
- Behavioral techniques such as biofeedback therapy
Here at Eggert Family Dentistry, Dr. Jeff and Dr. Elizabeth screen for evidence of bruxism during our exams. If your teeth indicate any damage from grinding, we’re here to partner with you in resolving the problem. Likewise, if you’re experiencing any symptoms that could indicate bruxism, such as jaw pain and stiffness, chronic headaches and more, be sure to let us know so we can help you overcome this destructive and uncomfortable activity.
Prolonged teeth grinding or clenching has the potential to damage your teeth irreversibly, so it’s worth taking every possible measure to overcome bruxism and to mitigate its erosive effect on your teeth. We look forward to helping you overcome bruxism and enjoy healthy teeth and reduced jaw and facial tension. Call us today at 651.482.8412 to schedule your next appointment.








 The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck.
The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck. A
A 
 When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others:
When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others: Did you know that, in
Did you know that, in  Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.


 Sleep apnea
Sleep apnea If a patient comes into our office with jaw pain, Dr. Elizabeth or Dr. Jeff evaluate many things, including the patient’s teeth and jaw. Because sinus problems can be a contributing factor to teeth and jaw discomfort, if their examination is inconclusive, Dr. Elizabeth or Dr. Jeff will refer our patient to an ENT for further evaluation.
If a patient comes into our office with jaw pain, Dr. Elizabeth or Dr. Jeff evaluate many things, including the patient’s teeth and jaw. Because sinus problems can be a contributing factor to teeth and jaw discomfort, if their examination is inconclusive, Dr. Elizabeth or Dr. Jeff will refer our patient to an ENT for further evaluation.