By: Dr. Elizabeth Eggert
Technology is constantly evolving.
We can see this in every area of life: from the cars we drive to the ways we communicate; things have changed quickly in our lifetimes. Even family movie night looks much different now than it did just a few decades ago!
Technology in the dental field has significantly evolved as well. We have vastly more powerful tools at our disposal than we once did, which has translated to much more efficient and effective dental care.
In this blog, we’ll explore why technology is important to your dental health and introduce some of the equipment you can expect to see used in the Eggert Family Dentistry office.
Why Is Dental Technology Important?
Dentists and patients alike benefit from advances in dental technology. Updates to procedures, treatments, and instruments make it easier for dentists to identify and address problems and improve outcomes for patients.
Modern technology has improved oral health in many ways. For example, Dr. Jeff Eggert and Dr. Elizabeth Eggert can identify and treat dental problems more effectively and conveniently than ever before. And patients benefit from a wider range of available treatment options as well as more efficient, less painful procedures.
At Eggert Family Dentistry, we are proud to provide improved treatment options using a number of technological advances in our clinic.
The Technology We Use at Eggert Family Dentistry
We routinely use advanced technologies in our offices including the iTero scanner, the Primescan with CEREC, digital x-rays, intraoral cameras, and electric handpieces. Here is a little more about these advancements and how they help us provide you with the best in oral care.
iTero Scanner

The iTero Element 5D Plus Lite is an intraoral scanner that gives us a fast, high-definition color 3D image of a patient’s mouth.
An intraoral scanner consists of a handheld camera wand, a computer, and software. Here’s how it works:
- We use the wand to scan your mouth, gently moving it over the surface of the teeth and gums.
- The iTero captures the size and shape of each tooth and displays a real-time 3D image on a touch screen.
- This image can be magnified and manipulated to enhance details in the areas we want to examine more closely.
- If appliances are needed, we can send the necessary scan information directly to the lab.
- iTero is perfect for scanning for Invisalign cases. In fact, this is why we invested in the iTero scanning unit, because we started doing so many Invisalign cases, it was much more convenient for everyone to use the scanner.
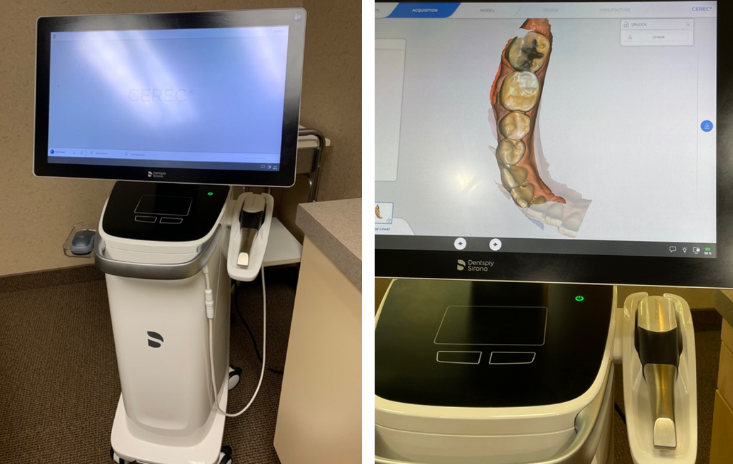
Primescan and CEREC

We have been using the Primescan with CEREC in our office for a number of years. This equipment allows us to create restorations like full crowns, inlays, onlays, and veneers right in our office…in a matter of minutes.
Traditionally, when you need a crown, it has always involved two appointments. The first is to prepare the tooth for the crown, take an impression of the tooth to have the crown made, and attach a temporary crown. Then, at the second appointment, the temporary crown is removed and the customized crown is permanently affixed.
With Primescan and CEREC, we are able to condense all of this down into one visit.
First, we’re able to take a digital impression of the tooth (rather than using the traditional putty method). Then, we can create your customized restoration while you wait and affix it right away. There’s no need for a temporary crown or to come back for a second appointment. We are proud to say that we are able to fabricate over 85% of our crowns at Eggert Family Dentistry using this one-visit method.
Digital X-Rays

Digital x-rays allow us to instantly take x-rays of your teeth to gather the information we need to quickly determine treatment and procedure options.
With the digital x-ray, we take an image of your teeth and view it in an imaging program. That program contains a number of tools that allow us to take a close look at your teeth and surrounding structures with incredible accuracy.
What’s more, the digital x-ray also uses nearly 80% less radiation than a standard x-ray, making it much safer for you.
Intraoral Camera
 An intraoral camera is a diagnostic tool that enables us to view different angles in the mouth that are difficult to see with a hand mirror. We use an intraoral camera to take photos of your teeth and gums and to show you any problem areas in your mouth. It is a great education tool!
An intraoral camera is a diagnostic tool that enables us to view different angles in the mouth that are difficult to see with a hand mirror. We use an intraoral camera to take photos of your teeth and gums and to show you any problem areas in your mouth. It is a great education tool!
The camera allows us to view the entire mouth on a monitor so we can get a closer look at any potential issues or problems that may arise and treat things before they become more serious. In addition, you are able to see for yourself what we are seeing in your mouth.
Electric Handpieces
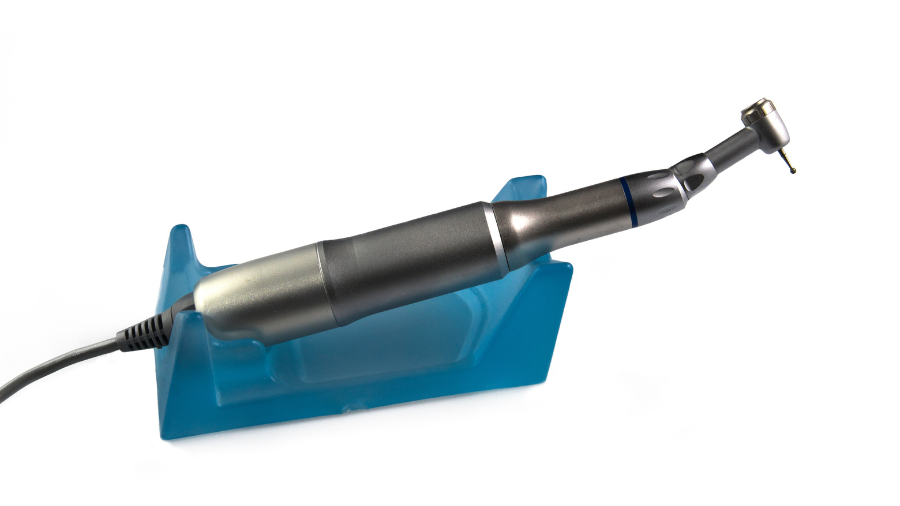
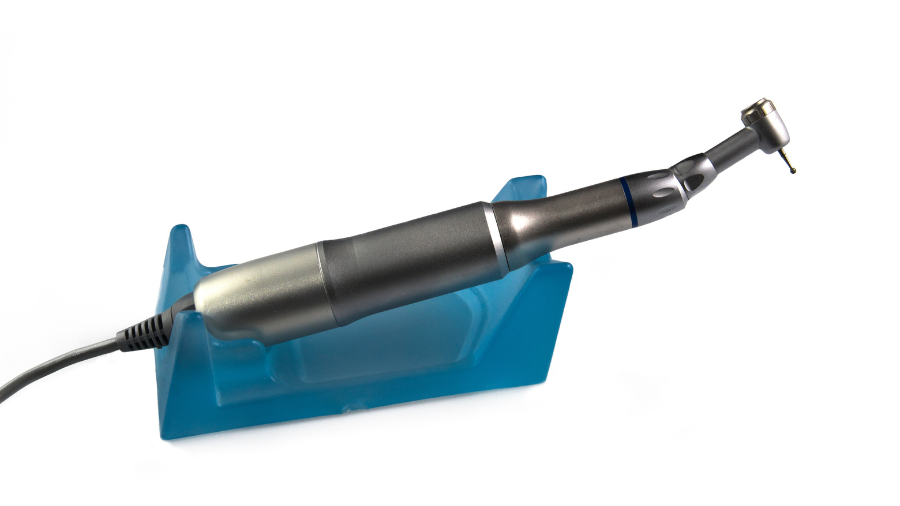
There are two types of handpieces commonly used in dentistry: air-driven handpieces and electric ones.
Electric handpieces are much stronger than air-driven ones because a motor spins the bur rather than air. This allows us to remove decay more quickly, reducing the time you need to be in the dental chair.
One example of where electric handpieces provide a great deal of benefit is in performing root canals. In Rotary Endodontics, we use a specialized electrical handpiece to perform a root canal, making the process faster and more effective and allowing us to perform the procedure with greater ease.
Enjoy a Better Dental Experience Thanks to Technology and Eggert Family Dentistry

At Eggert Family Dentistry, our patients enjoy efficient, successful, and more comfortable procedures thanks to the latest in dental technology, along with the compassionate care of Dr. Jeff Eggert and Dr. Elizabeth Eggert.
No matter your dental needs, Dr. Jeff Eggert or Dr. Elizabeth Eggert will use their expertise to evaluate your oral health and determine the best treatment options for you. Contact our office in North Oaks, MN at 651-482-8412 to schedule an appointment today.




 An intraoral camera is a diagnostic tool that enables us to view different angles in the mouth that are difficult to see with a hand mirror. We use an intraoral camera to take photos of your teeth and gums and to show you any problem areas in your mouth. It is a great education tool!
An intraoral camera is a diagnostic tool that enables us to view different angles in the mouth that are difficult to see with a hand mirror. We use an intraoral camera to take photos of your teeth and gums and to show you any problem areas in your mouth. It is a great education tool!