By: Dr. Elizabeth Eggert
If you’ve found yourself constantly sniffling, sneezing, or feeling congested lately, you’re not alone. Spring and early summer are peak times for seasonal allergies, as pollen levels surge in the air. According to the Centers for Disease Control and Prevention (CDC), around 25% of adults and nearly 19% of children in the United States suffer from seasonal allergic rhinitis—commonly known as hay fever. This increase in allergens can make breathing through your nose a daily struggle, but the good news is, you have several effective options to help clear your nasal passages and breathe more easily.
What Are Your Triggers?
The first step to improving nasal breathing is identifying your triggers. Pollen from trees, grasses, and weeds is one of the most common culprits this time of year. If you know you’re allergic to certain types of pollen, it’s helpful to track local pollen forecasts and try to stay indoors when counts are high—typically in the early morning or on windy days. Keeping windows closed and using an air purifier can also help minimize exposure indoors. By reducing your contact with allergens, you make it easier for your nose to stay clear and function normally.
What Can Be Done For The Nose?
One of the simplest and most natural ways to combat nasal congestion is to use a saline nasal spray every day. These sprays can even be used multiple times a day to rinse allergens and irritants out of your nasal passages. They’re non-medicated and safe for regular use, making them a great first line of defense. For a deeper clean, consider using a neti pot—a small device that flushes warm saline solution through your nasal cavity. Just be sure to use distilled or sterile water and clean your device after each use to avoid introducing bacteria.
If saline sprays and rinses aren’t enough, you may benefit from over-the-counter allergy medications. Nasal corticosteroids like Flonase (fluticasone) are particularly effective at reducing inflammation inside your nasal passages. When used daily during allergy season, these medications can significantly improve your ability to breathe through your nose. Antihistamines like cetirizine or loratadine can also help, especially if you have other symptoms like itchy eyes or sneezing. Be sure to talk to your doctor about what options might be best for you!
Why Breathing Through Your Nose Is So Important?
Improving your nasal breathing isn’t just about comfort—it’s also important for your overall health. Breathing through your nose helps filter, humidify, and warm the air you inhale, which can reduce your risk of respiratory infections and improve sleep quality. When nasal congestion forces you to breathe through your mouth, you may experience dry mouth, snoring, and even disrupted sleep patterns, leaving you feeling groggy and irritable during the day. From a dental perspective, we also see a lot more decay and periodontal disease in patients that breathe through their mouths because the saliva is affected and diminished.
By staying proactive and using the right combination of strategies—whether it’s saline rinses, allergy medication, or avoiding high-pollen environments—you can take control of your nasal health. As allergy season ramps up, don’t wait until you’re completely congested to act. Start incorporating these tools into your daily routine now, and you’ll be breathing easier in no time.
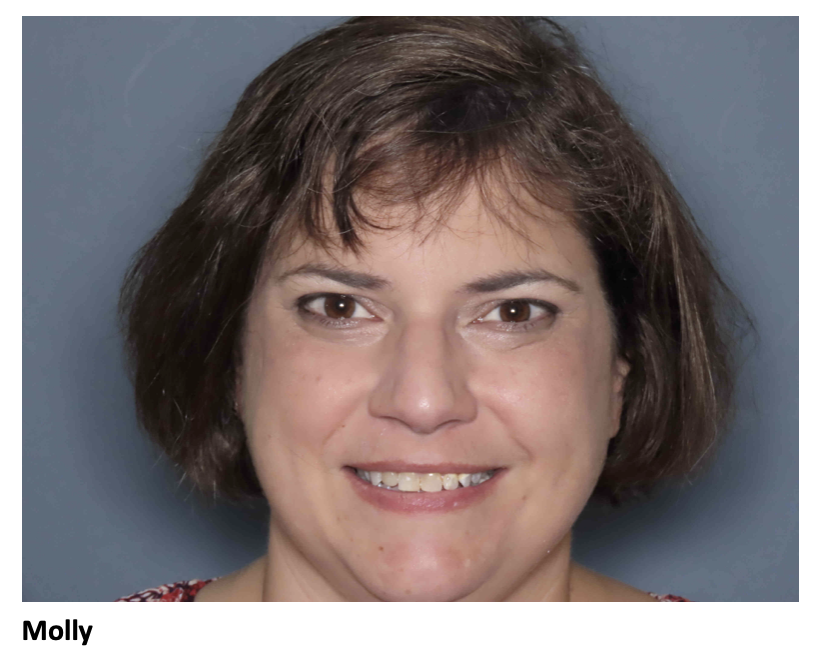
Why Do We Care?
At Eggert Family Dentistry in North Oaks, MN, our goal for all our patients is whole-body, overall health. We see patients every day who struggle to breathe through their noses. This not only makes their dental treatments more difficult, but keeps our patients from obtaining their ultimate health. We coach patients on breathing techniques and can make suggestions specific for you. We also have adjunctive services like Nitrous Oxide (Laughing) Gas and myofunctional exercises we can suggest to improve your ability to breathe through your nose. Call us today at 651.482.8412 and come in for your customized comprehensive exam! We look forward to helping you improve your health!