By: Dr. Elizabeth Eggert
Obstructive sleep apnea (OSA) is a condition that must be taken seriously. Obstructive sleep apnea is an airway blockage that occurs when, during sleep, muscles in the back of the throat relax and/or the tongue and surrounding tissues migrate back into the throat, obstructing the airway.
Not only can sleep apnea cause fatigue, headaches and memory loss but it can also lead to even more serious health issues such as hypertension, heart failure and stroke.
Many people don’t understand what causes sleep apnea and how it affects oral health. We’re going to take a few minutes to unpack some of these connections.
Risk factors for sleep apnea
 When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others:
When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others:
- Over 40 years of age
- Obesity
- Large tongue or tonsils
- A large neck
- A small jaw
If we think you might be dealing with an airway issue like sleep apnea, we’ll ask you if your loved ones complain that you snore or gasp for air when you sleep. We’ll ask you if you deal with insomnia or daytime drowsiness. Do you wake up with a headache or a dry mouth? Do you have nasal or sinus problems?
We will also look for signs of TMD, bruxism or dry mouth, all of which can be connected to OSA.
TMD goes hand in hand with sleep apnea
 Did you know that, in 52% of obstructive sleep apnea cases, a person also struggles with temporomandibular disorder or TMD?
Did you know that, in 52% of obstructive sleep apnea cases, a person also struggles with temporomandibular disorder or TMD?
TMD occurs when the temporomandibular joint (TMJ) doesn’t function properly. When the joint is irritated, chewing and talking can be mildly to moderately painful.
So why do sleep apnea and TMD often occur together? When a person is deprived of oxygen during sleep, their body will compensate in unconscious ways. In many cases, their jaw muscles clench and release or grind the jaw around to gain more airway space. When sleep apnea is left untreated, this jaw motion becomes habitual and can cause TMD or even deterioration of the jaw joint itself.
Bruxism goes hand in hand with sleep apnea
 Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
Symptoms of bruxism include broken, cracked, chipped or worn teeth. Because the clenching and grinding of teeth cause tension in a person’s head, jaw and muscle discomfort are commonly present.
Of the 31% of adults who deal with bruxism, at least 25% of them also battle OSA.
Sleep apnea leads to mouth breathing
As we already stated, sleep apnea is an airway obstruction often caused by soft tissues that move towards the back of the mouth during sleep. In addition to clenching and contracting your jaw muscles in response, a person will typically also mouth breathe in an attempt to get more oxygen.
Mouth breathing leads to snoring but it also leads to other, more serious oral consequences.
Saliva plays an important role in rinsing food and harmful bacteria out of our mouths. When a person breathes through their mouth, it becomes dry and becomes a haven for food particles and bacteria. Without this natural “rinsing” function, plaque easily grows under the gumline and can cause tooth decay, gingivitis and in extreme cases, periodontal disease.
If you’re experiencing symptoms of sleep apnea or related conditions, Dr. Elizabeth or Dr. Jeff would love to see you in our office. They can evaluate your situation, determine which factors are present and, if they see evidence of sleep apnea, refer you to your primary doctor who may refer you to an ENT or sleep specialist. Then Dr. Elizabeth or Dr. Jeff will partner with these specialists to determine the best courses of action to help alleviate sleep apnea and any peripheral issues and restore your health. Schedule your appointment by calling our office at 651.482.8412!




 Candy on a stick, such as lollipops or rock candy, is meant to be enjoyed over time. Because it lingers in your mouth, it increases the production of saliva. However, instead of the saliva doing its job and rinsing bacteria out of your mouth, it only spreads the sugar around. Additionally, your mouth produces acid in an attempt to destroy the sticky sugar that then coats your teeth. The acid and sugar team up to break down tooth enamel and, with repeat exposure, can result in tooth decay.
Candy on a stick, such as lollipops or rock candy, is meant to be enjoyed over time. Because it lingers in your mouth, it increases the production of saliva. However, instead of the saliva doing its job and rinsing bacteria out of your mouth, it only spreads the sugar around. Additionally, your mouth produces acid in an attempt to destroy the sticky sugar that then coats your teeth. The acid and sugar team up to break down tooth enamel and, with repeat exposure, can result in tooth decay. You might be wondering where sour candy fits into the picture. Warheads, Sour Patch Kids, Sour Skittles…kids LOVE sour candy and love to challenge themselves and their friends to eat large quantities of it or hold the sour candy in their mouths for long periods of time.
You might be wondering where sour candy fits into the picture. Warheads, Sour Patch Kids, Sour Skittles…kids LOVE sour candy and love to challenge themselves and their friends to eat large quantities of it or hold the sour candy in their mouths for long periods of time. One of the most popular categories of Halloween candy are chocolates. While many have sticky centers like Twix, Rollos or Snickers, others like Hershey’s bars and Nestle Crunch dissipate quickly in your mouth, making them more dental-friendly than almost any other candy.
One of the most popular categories of Halloween candy are chocolates. While many have sticky centers like Twix, Rollos or Snickers, others like Hershey’s bars and Nestle Crunch dissipate quickly in your mouth, making them more dental-friendly than almost any other candy.
 When you bring your baby in for their first dental visit, Dr. Elizabeth or Dr. Jeff will take a peek in their mouth and check all erupted teeth to make sure they’re healthy. Then they will discuss basic baby and toddler oral care, address the
When you bring your baby in for their first dental visit, Dr. Elizabeth or Dr. Jeff will take a peek in their mouth and check all erupted teeth to make sure they’re healthy. Then they will discuss basic baby and toddler oral care, address the 
 Buy your child a new toothbrush, a tube of
Buy your child a new toothbrush, a tube of  Check the school’s gum policy and, if it’s allowed, give your child a pack of sugar-free gum to chew after lunch to help clean their teeth
Check the school’s gum policy and, if it’s allowed, give your child a pack of sugar-free gum to chew after lunch to help clean their teeth Crunchy foods like carrots, celery and apples; limit citrus fruits which erode enamel quickly
Crunchy foods like carrots, celery and apples; limit citrus fruits which erode enamel quickly Put a travel toothbrush, a small tube of fluoride toothpaste, a container of floss and a container of dental wax in a small zipper bag and encourage them to brush their teeth after lunch
Put a travel toothbrush, a small tube of fluoride toothpaste, a container of floss and a container of dental wax in a small zipper bag and encourage them to brush their teeth after lunch



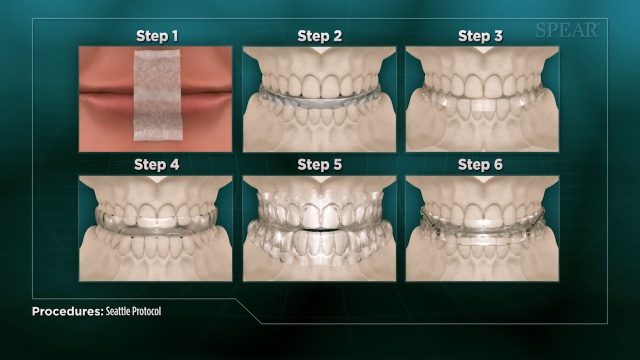
 The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck.
The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck. A
A 
 When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others:
When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others: Did you know that, in
Did you know that, in  Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.