By: Dr. Elizabeth Eggert
The quality of our sleep can make or break the day ahead. There’s nothing like a clear head and boatloads of motivation after a solid night’s sleep! Consistent, quality sleep can set us up for success in all aspects of life. Conversely, over time, poor sleep can take a toll—affecting our focus, job performance, relationships, and overall well-being. Surprising to many, dental interventions like the Seattle Protocol and oral sleep appliances are often the key to better sleep. Read on to learn more!
Understanding Sleep-Disordered Breathing
Just because your head is on your pillow for 7-9 hours at night, you’re not guaranteed solid sleep. If you’re waking up feeling tired and you’re fighting daytime fatigue, you may be struggling with sleep-disordered breathing.
Sleep-disordered breathing (SDB) encompasses a range of conditions that interfere with normal airflow during sleep. The most commonly understood form of SDB—sleep apnea—occurs when the airway becomes partially or completely blocked, often due to the jaw’s position or relaxed throat muscles and tissues. Symptoms can include loud snoring, gasping for air, morning headaches, dry mouth, and daytime fatigue, among others. There are many other patterns of sleep disordered breathing that aren’t as extreme as sleep apnea, but can still cause you to get poor quality sleep. Working to address any SDB is beneficial to your overall health.
The Role of Dentists in Treating Sleep Apnea
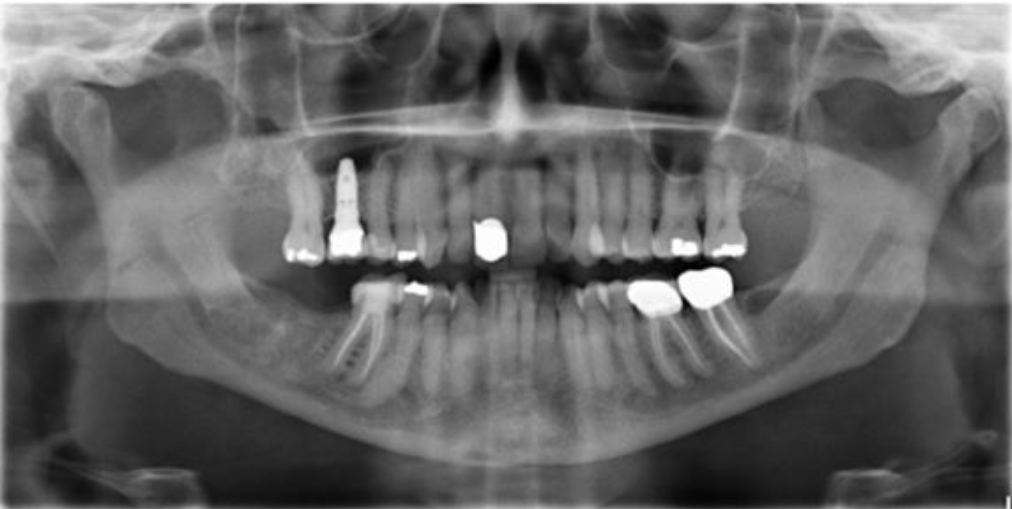
You might not expect your dentist to be the one to help with sleep issues, but they’re actually in a unique position to identify and treat sleep disordered breathing, including sleep apnea. At Eggert Family Dentistry, we specialize in evaluating the structure and function of your jaw and airway, as well as the status of your teeth, to determine whether they may be contributing to sleep dysfunction.
The Seattle Protocol and Its Benefits
So where does it all begin? The Seattle Protocol is a six-step process that helps patients with symptoms of sleep-disordered breathing and other conditions to determine whether a compromised airway is causing their ailments.
Each of the six steps builds upon the last to open the airway as much as possible, but patients don’t necessarily need to complete the entire process to identify their best solution. The purpose of the protocol is to determine which step provides the patient with the most relief of symptoms.
The Six-Step Seattle Protocol Process:
- Nose Breathing and Mouth Taping: During this stage, you will gently train your body to breathe through your nose, not your mouth.
- Temporary Splint for Lower Jaw and Mouth Taping: Once you’ve adjusted to the mouth taping, the second step of the protocol adds a temporary splint for your lower jaw while you sleep.
- Temporary Splint for Lower Jaw with Lower Jaw Pulled Forward and Mouth Taping: If adding the lower splint only isn’t giving you the restful sleep you deserve, we add an element that holds your lower jaw forward.
- Temporary Splint for Lower and Upper Jaw with Mouth Taping: If you aren’t getting relief from the previous step, we remove the forward jaw posturing component and add a splint for your upper jaw.
- Temporary Splint for Lower and Upper Jaw with Lower Jaw Pulled Forward and Mouth Taping: If you need to continue in the protocol, step five again adds a horizontal component by linking the upper and lower splints together and moving the lower jaw forward.
- Temporary Splint for Lower and Upper Jaw with Lower Jaw Progressively Pulled Forward and Mouth Taping: If you still aren’t getting that good night’s sleep, we move to the final stage of the Seattle Protocol. In this stage, we keep moving your lower jaw forward incrementally until you feel well-rested.
Once they gather information from the Seattle Protocol—and if they determine that sleep-disordered breathing is a factor for you—Dr. Elizabeth Eggert and Dr. Jeff Eggert can create a custom night guard or splint or sleep appliance that opens up your airway and curbs any inflammation or damage to your teeth, jaws, or soft tissue. These custom-fit devices gently reposition the jaw to keep the airway open while you sleep—reducing snoring and improving oxygen flow. These appliances are non-invasive, convenient, and generally more comfortable than a CPAP machine.
At Eggert Family Dentistry, our ultimate goal is to help you reclaim the rest your body and brain need to thrive.
Are You Struggling With Sleep?
Be mindful of your symptoms. Take note of how often you feel fatigued, whether you snore, or if you wake up frequently during the night. It’s also helpful to ask your partner about any sleep habits they’ve noticed. Partners often detect signs of sleep apnea or other disturbances that may go unnoticed by the person experiencing them. And, partners aren’t always willing to share what they know about your sleep habits unless you ask, since they don’t want to hurt your feelings!
Next, schedule a consultation with Eggert Family Dentistry. We’ll assess your symptoms and explore whether sleep-disordered breathing could be the underlying issue. If it is, we’ll work with you to create a customized treatment plan. Professional solutions, such as a tooth-based appliance or other interventions, can even contribute to better overall health.
You don’t have to suffer from inferior sleep. Give us a call at 651.482.8412 to set up your appointment with Dr. Elizabeth Eggert or Dr. Jeff Eggert and see if dentistry holds the key to unlocking the key to better sleep for you!