By: Dr. Elizabeth Eggert
How did this start?
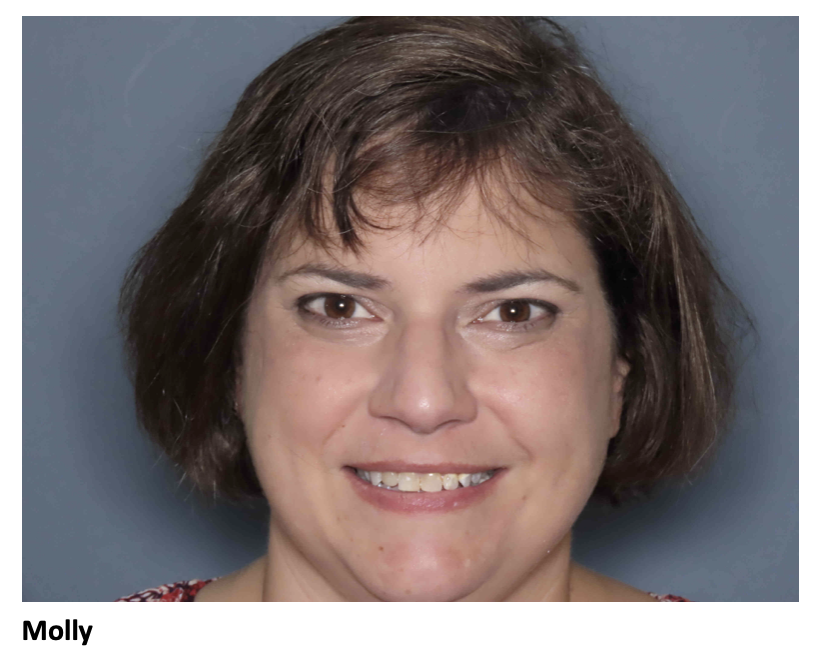
ML (name withheld by request of patient) has been a patient of Dr. Elizabeth Eggert for over 10 years. When ML first came as a patient, Dr. Elizabeth had been working to do a complete oral reconstruction for his mother. His mom urged him to seek Dr. Elizabeth’s council as she was concerned for the long-term health of his teeth. When ML came to us, he mentioned that he knew he had a lot of tooth wear. In interviewing ML, he noted he had difficulty sleeping and said it would take up to 45 minutes for him to fall asleep. He also didn’t think he had a stable bite, despite being in orthodontics on and off for 14 years of his childhood and teenage years. He did have 4 teeth extracted for his first orthodontic treatment (2 upper bicuspids and 2 lower bicuspids). You can note from the BEFORE photos that ML had tooth wear and his upper teeth were stuck inside his lower teeth – this is a condition called “crossbite.”

What was recommended?
ML went through the Records Process and it was determined that the wear on his teeth was increasing at an accelerated rate and the current position of his teeth would put them at high risk for continued wear, chipping, cracking, breaking, and potentially even tooth loss. The recommendations were to get ML’s teeth into a more idealized position, keep bone support for the teeth, and restore the teeth where they have worn in order to build back to normal tooth proportions.
Years ago when ML underwent orthodontics for the first time, we didn’t know as much as dental professionals about airway and jaw constriction. It was fairly common for patients like ML to undergo extractions in order to “gain space” and “alleviate crowding.” We know more now as a profession about how this affects sleep, breathing, and tooth wear over time. Instead of extractions to “gain space” it is much more common now to encourage the bones to grow into positions that can support all the teeth. We are much more likely to recommend expansion or expanders. This solution works very well in growing children. As an adult, this was still possible for ML, but would require jaw surgery to make the corrections. Therefore, orthodontics, jaw surgery, and restorations were recommended for ML. Dr. Elizabeth also talked to ML about the alternative treatment of restoring all of his teeth and rebuilding to a different bite, but ML wanted to limit the number of restorations and Dr. Elizabeth told ML that she preferred to see a wider arch for his teeth anyway.
What did ML want?
“My lifetime goal for my teeth is to keep them.” He reported he has never been happy with the appearance of his teeth. He didn’t want “nuclear” white teeth, but he said if he was going to improve his bite, he wanted his teeth to look nicer too. ML started the process with Dr. DeVoe (orthodontist) to change his bite without any surgical correction. Dr. DeVoe did a nice job improving ML’s crossbite and moving the teeth into a position where restorations could be done to rebuild tooth proportions.
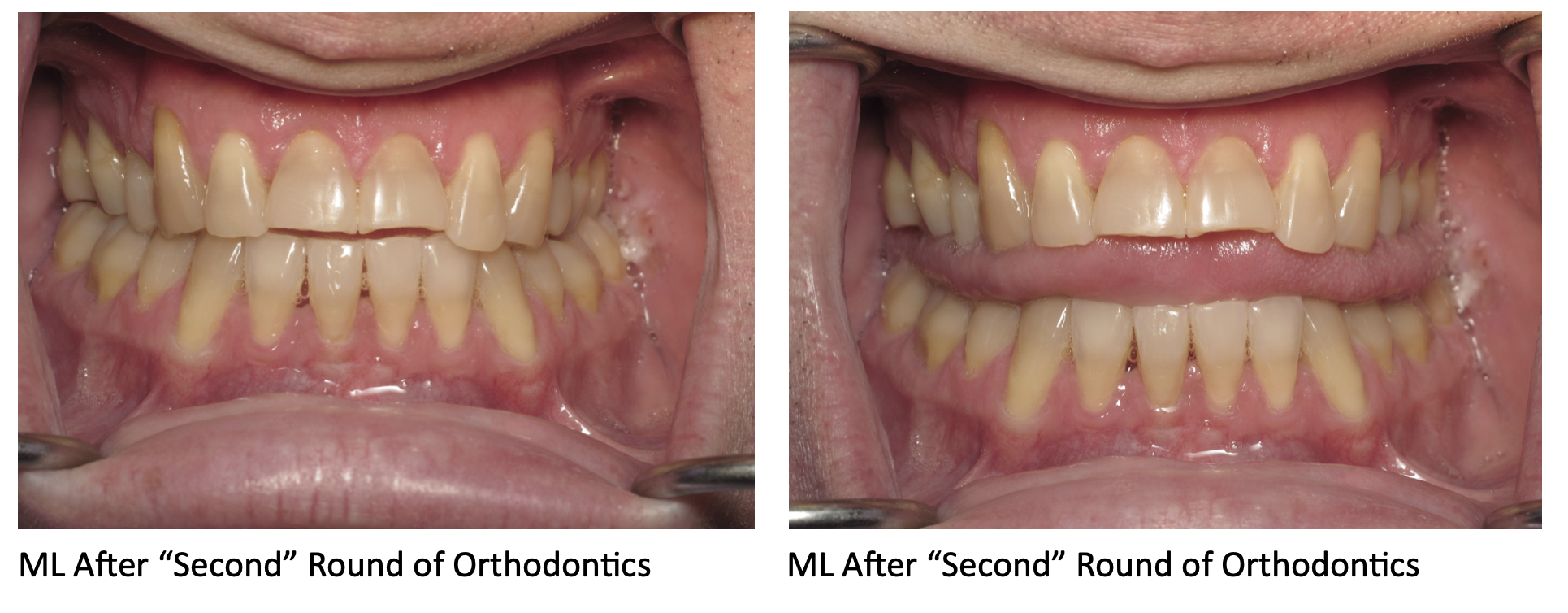
However, even after this second round of orthodontics (ML’s first round as an adult), it was still difficult to even out his bite forces without doing a large number of restorations. Also, there was an “elephant in the room:” ML’s tongue. Dr. Elizabeth couldn’t help but notice how much space ML’s tongue wanted. As you can see in the photo above, ML’s tongue wanted lots of room and would spill over his teeth with his teeth apart. It was also always very visible in photos and very active when working on ML.
While doing the consultation after this second round of orthodontics, ML said “Well, there is always still the option of jaw surgery.” While ML had not been set up orthodontically for jaw surgery, Dr. Elizabeth told ML that he was correct, there still was that option, if he was willing to undergo more orthodontics. She also shared with him the story of her mom’s journey with jaw surgery and orthodontics.
What was involved?
ML went back into orthodontics. He had 2 different surgeries with Dr. Andreasen of Momenta Oral Surgery. One to open his upper arch and expand that space and another to move his upper and lower jaw bones forward. This extended his treatment time frame, but after this third round of orthodontics, he was ready for restorations. ML felt his teeth were disappearing, it was time to rebuild them back to visible proportions.

It is easy to see how ML’s oral space improved after his jaw surgeries. His tongue is happy to have so much more room! For color and tooth proportion corrections, Dr. Elizabeth recommended a minimum of 14 restorations (8 upper teeth and 6 lower teeth) along with equilibration to finalize the bite. ML wanted whiter teeth, but it was decided that since he was doing 14 restorations, his back teeth wouldn’t show in his smile so bleaching was not needed before the restorations were done. Therefore, we did a wax-up so ML could see what the final restorations would look like and after he approved the wax-up, we prepared the teeth for restorations and a few weeks later seated his restorations.
What does he think?
When we asked ML what he thought about doing the procedure before we started he stated, “This was necessary; I never saw this as elective, but I wasn’t really looking forward to it. The thought of something happening to my teeth was a little uncomfortable. I don’t think anybody likes doing something to their body that is irreversible.”
However, ML is very happy he completed the procedures and ended up doing the jaw surgeries after all. He is surprised at how much bigger his airway is and that he no longer makes sounds at night when sleeping. He always believed he could not breathe through his nose because of allergies, but that does not seem to be the case after this treatment, it appears that he needed expansion of his oral spaces. (Note there is NO tongue visible in ML’s AFTER photo.) ML says it was a long road and he learned a lot along the way, but it was necessary!
Congratulations on your amazing results ML and thank you for putting your trust in us! We were delighted to help you through this journey!