By: Dr. Elizabeth Eggert
Most teenagers are averse to the taste and smell of cigarettes, and we’ve seen a sharp decline in cigarette use among teens in recent decades (it’s helped that smoking cigarettes has fallen “out of style”). However, the lure of smoking is still just as strong as it was in the 20th century – it just looks a little different.
E-cigarettes or “vapes” are electronic devices that heat nicotine and disperse it as an aerosol. There is no smoke or tobacco involved, so many teenagers have been led to believe that vaping isn’t as bad for you.
Regardless of whether or not they realize it, the #1 problem of vaping is still the exact same as smoking: Nicotine is one of the most addictive chemicals on the planet.
At Eggert Family Dentistry, our patient’s health and well-being are our top priority, and we are here to support you in any way we can. Here’s what you and your teenager need to know about vaping.
Who’s Vaping and Why?
A 2022 study released by the U.S. Food and Drug Administration (FDA) and the U.S. Centers for Disease Control and Prevention (CDC) found that 2.55 million U.S. middle and high school students reported current e-cigarette use in 2022. That number represents 14.1% of high school students and 3.3% of middle school students.
Students vape because of three main reasons:
- Many teens believe vaping is less harmful than smoking.
- E-cigarettes have a lower per-use cost than traditional cigarettes.
- Youths and adults find the lack of smoke appealing. With no smell, e-cigarettes reduce some of the stigma of smoking.
It’s true that vaping is thought to be less harmful to the lungs than inhaling smoke, however, research is still being done and due to all the chemicals involved with e-cigarettes, the evidence isn’t clear. However, if this is the reason your teen cites to defend their vaping addiction, tell them that it’s also true that knives are less harmful than guns. That said, we still wouldn’t want to be faced with either.
Additionally, nicotine as an aerosol comes with its own serious health risks — not only does the vapor contain a known pesticide, but there are hundreds of chemicals present in aerosols that have yet to be identified. We don’t yet know all the side effects and risks.
Side Effects and Dangers of Vaping
What we know for sure is that E-cigarettes contain harmful chemicals such as:
- Formaldehyde, which is known to cause cancer.
- Acrolein which is used as a weed killer and can cause irreversible lung damage.
- Flavorants such as diacetyl, a chemical linked to serious lung disease.
- Volatile organic compounds such as benzene, which is found in car exhaust.
- Heavy metals, such as nickel, tin, and lead.
- Nicotine, which is highly addictive and damaging to the brain.
Just like smoking, there are two sets of side effects when it comes to vaping. One category of side effects has to do with the physical act of inhaling chemicals/vapor into the lungs (vaping). The other category has to do with becoming a nicotine addict.
Side Effects of Vaping:
Because vaping is relatively new, researchers don’t yet know all the effects vaping can have on your body. What we do know, though, is alarming enough:
- Difficulty Breathing: The particles you inhale while vaping can cause inflammation (swelling) and irritation in your lungs, making it harder to catch your breath.
- Asthma: Vaping can make you more likely to get asthma and other lung conditions. It can also make your existing asthma worse.
- Lung Scarring: Diacetyl, a chemical used in some flavorings, can cause bronchiolitis obliterans (“popcorn lung”). Bronchiolitis obliterans causes permanent scarring in your lungs. That means that even if someone quits vaping, the negative effects of it will be with them for the rest of their lives.
Side Effects of Being a Nicotine Addict:
Any addictive substance is going to cause harm, but nicotine addiction can be especially harmful.
- Nicotine Dependency: When you start vaping, it only takes a few days of consistent use before your brain starts to rely on the presence of nicotine in order to feel normal. Without a constant supply, nicotine addicts go into withdrawal and feel anxious, stressed, unsettled, irritable, and fidgety.
- Inability to Focus: Nicotine is the one of the most addictive chemicals on the planet because it enters and leaves your system quickly, which is why smokers and vapers feel the need to smoke/vape every 20 minutes or so. This makes it noticeably more difficult to focus for prolonged periods of time. Whether you’re writing an essay, taking a test, drawing a picture, relaxing with friends, or watching a movie, so long as you are still vaping, your addiction will always make you feel the need to vape.
- Increased Anxiety: The popular belief is that smoking and vaping can calm you down. Researchers know that the exact opposite is true: Nicotine spikes your heart rate and blood pressure, which is directly responsible for increasing anxiety.
- Other Mood Disorders: Several studies have also found that nicotine addiction during adolescence is also associated with a higher risk of developing mental and behavioral problems during adulthood, including: major depressive disorder, agoraphobia, and panic disorder.
How Vaping Affects Your Oral Health
Nicotine, whether smoked or vaped, restricts blood flow to the gums, which can contribute to gum disease. The fluid in e-cigarettes only increases the risks. Other ways that nicotine and aerosol can harm your oral health include:
- Dry mouth: Nicotine in e-liquid inhibits saliva production which leads to dry mouth. When your mouth is dry, it’s a perfect habitat for bacteria which can lead to tooth decay.
- Damage to soft tissue/enamel: Propylene glycol is used as a carrier ingredient in e-liquid, propylene glycol has toxic effects on soft tissue and enamel. Additionally, e-liquid flavorings when added to vegetable glycerin cause a 27% decrease in the hardness and integrity of tooth enamel.
- Receding Gums: Continued nicotine exposure causes reduced blood flow which can cause gum tissue to die and recede, exposing more of the tooth.
- Tooth Decay/Loss: Exposed gums leads to tooth sensitivity, an increase in cavities, and in some cases, tooth loss.
The Bottom Line
Even if you believe your child would never use e-cigarettes or vapes, it’s important to talk to your teenager about vaping. Even those teens who manage to avoid peer pressure are still going to be exposed to vaping at some point in their lives. It’s important to make sure your child is prepared with the right information to make the correct decision.
Questions About Vaping and Your Oral Health?
Vaping poses significant risks to your oral and overall health. If you or a loved one are struggling to quit vaping or have any concerns about its effects on your oral health, please don’t hesitate to reach out to us at Eggert Family Dentistry. Dr. Jeff Eggert and Dr. Elizabeth Eggert are committed to providing comprehensive dental care to our patients and are happy to answer any questions you may have. Give us a call at 651-482-8412 to schedule an appointment today, or to learn more about how we can help you and your teen maintain a healthy, beautiful smile.










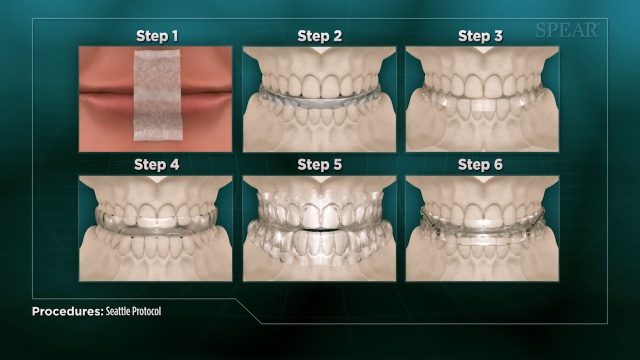

 The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck.
The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck. A
A