By: Dr. Elizabeth Eggert
Is one of your New Year’s resolutions to focus more on your dental health? If not, it’s never too late to make it a priority! If you focus on keeping your teeth and gums healthy, your overall well-being (and your wallet) will thank you.
So how can you improve your dental health this year? Well, a healthy smile goes beyond just brushing and flossing — it also involves regular dental check-ups and “recare” visits. Let’s take a look at why improving your dental health should be high on your list, various ways you can improve your oral health, and some examples of easy dental resolutions you can follow in 2024.
The Link Between Dental Health and Overall Health
As the new year unfolds, many of us make resolutions to lead healthier lives, the classic resolution being to hit the gym. And while many think exercise and nutrition are the end-all-be-all of health, the truth is that our body’s wellbeing is a result of many interconnected systems, each affecting the other. Your dental health, for example, can impact various aspects of your overall health, including cardiovascular health, respiratory health, and even mental health.
Oral health’s impact on the heart: Study after study has shown that people who have poor oral health (such as gum disease or tooth loss) have higher rates of cardiovascular problems such as heart attack or stroke than people with good oral health. Researchers have proposed many theories as to why this connection exists, including bacteria from the mouth traveling through blood vessels, inflammation causing an immune response, or the correlating factor of smoking cigarettes. Whatever the cause, the relationship between oral health and cardiovascular health has been demonstrated many times over.
Oral health’s impact on the lungs: According to research, oral health directly impacts incidences and outcomes of lung diseases, such as pneumonia and chronic obstructive pulmonary disease (COPD). In a healthy person, the lungs are usually able to fight off any bacteria that would accumulate in the mouth and travel through the respiratory system. However, when a person’s lungs are compromised by a pre-existing respiratory condition, the lung’s immune response is weaker. This makes it easier for bacteria that accumulates in an unclean mouth to travel to the lungs and cause infections.
Oral health’s impact on mental health: Studies since the COVID 19 pandemic have shown that mental health and oral health are correlated, with associations demonstrated between mental health problems and tooth loss, periodontal disease, and tooth decay. Dental decay and tooth loss can lead to more frequent pain, which often increases social isolation, and feelings of low self-esteem. All of this results in a lower quality of life, which often leads to poorer mental health.
Poor oral hygiene can have a domino effect on multiple systems of the body. By resolving to improve your dental health in 2024, you’re not just preserving your smile – you’re protecting the wellbeing of your entire body.
The Importance of Regular Recare Visits
Most people understand that brushing twice and flossing once daily are the pinnacles of good oral health. However, it’s equally important to schedule regular dental appointments, also known as recare visits — it is important to realize that these visits are much more than “just a cleaning.” It is essential to be committed to them and never skip out! When scheduled regularly, these appointments play a key part in preventing and detecting dental problems early on.
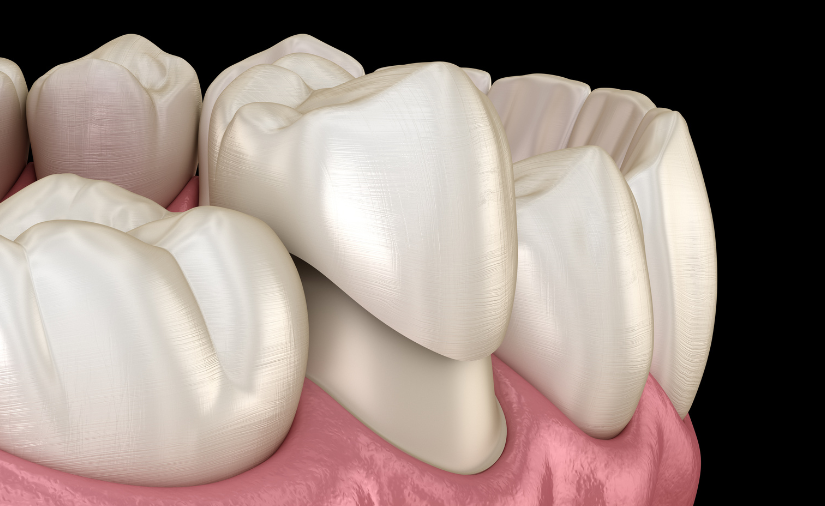
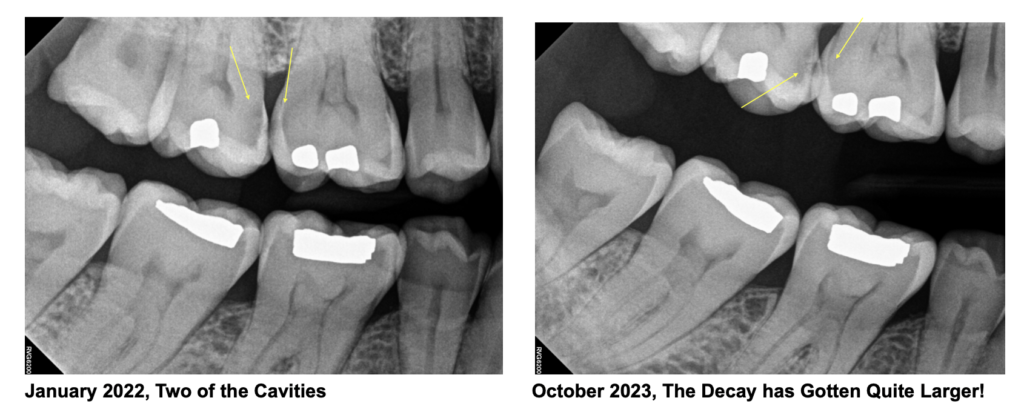
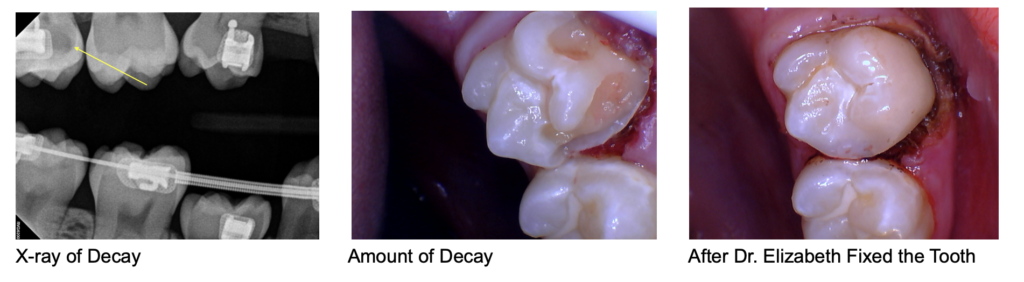
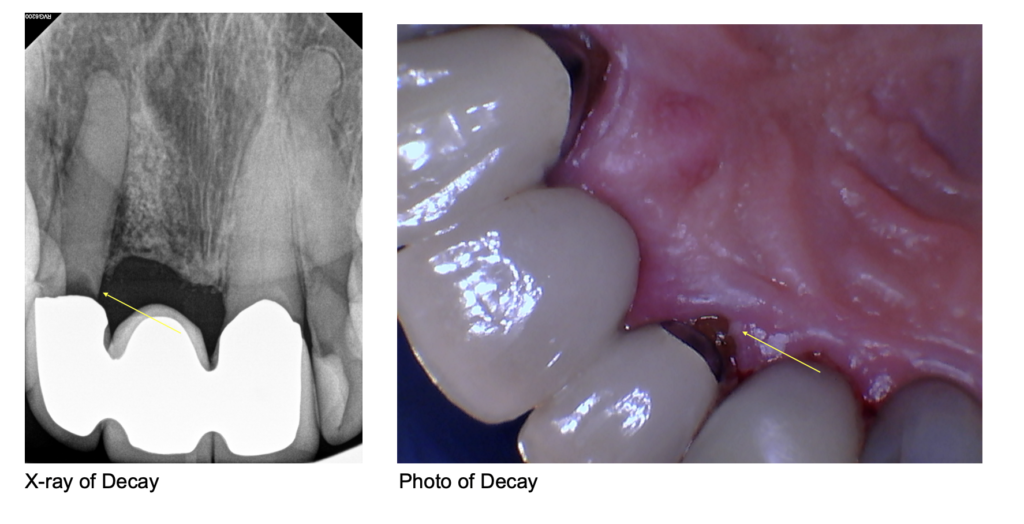
When you schedule a recare appointment with Eggert Family Dentistry, Dr. Jeff Eggert or Dr. Elizabeth Eggert can make sure that small problems like gingivitis and cavities don’t escalate into more significant (and expensive) issues, such as periodontal disease and tooth loss. When you come in for your appointment, not only will you get a professional teeth cleaning, but you’ll also receive a thorough check-up to ensure the health of your mouth and the quality of any dental restorations/devices such as fillings, crowns, dentures, or veneers.
Questions? Call Eggert Family Dentistry
Your smile is an essential part of your overall health, and when you prioritize your dental health, you’re investing in a lifetime of well-being. Call Eggert Family Dentistry at 651.482.8412 to schedule your recare appointment today or to ask any questions you have about dental health. Make 2024 the year you take charge of the health of your smile – your future self will thank you!


























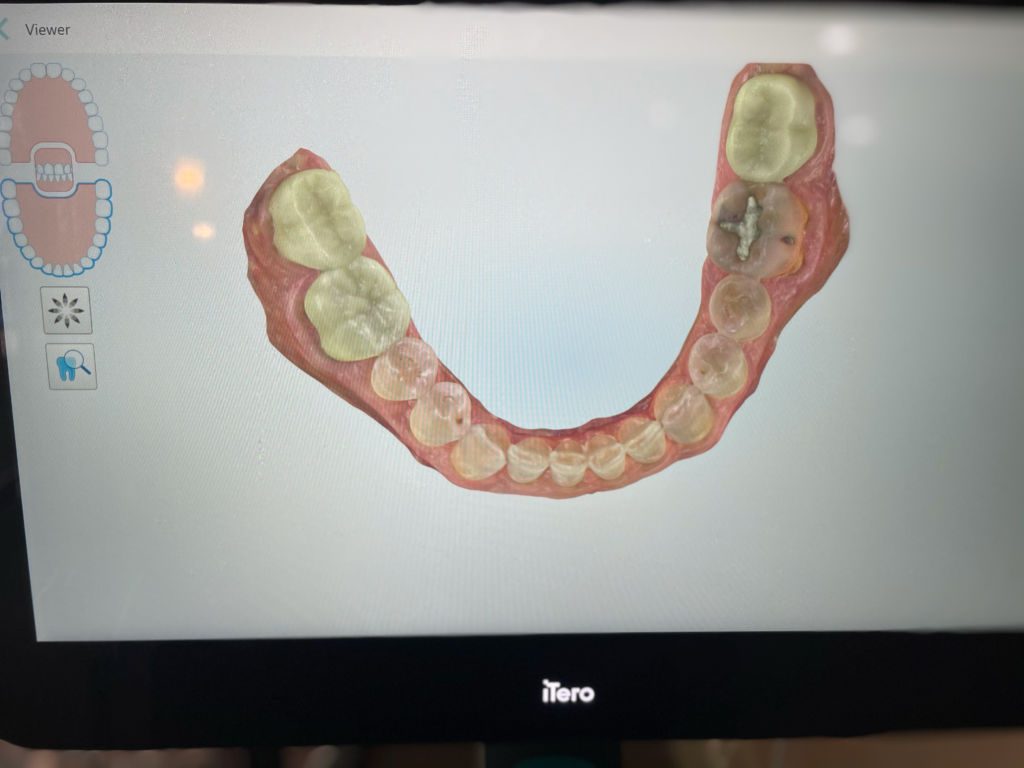
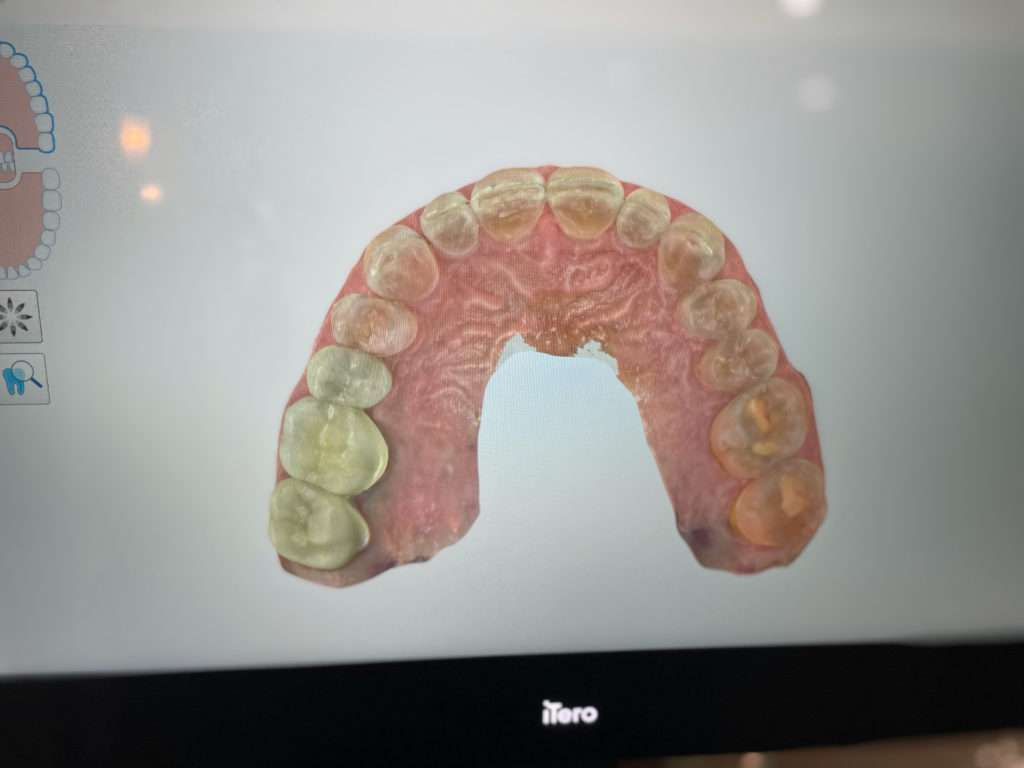
 Traditional dental impressions were once synonymous with discomfort, gooey molds, and anxious waiting. Fortunately, times are changing. Dental scanning units, like the iTero, are starting to change the way we are able to approach dental care. Dr. Elizabeth and Dr. Jeff are now able to use these state-of-the-art scanning units to complete your care, helping to make the patient experience smoother and more precise.
Traditional dental impressions were once synonymous with discomfort, gooey molds, and anxious waiting. Fortunately, times are changing. Dental scanning units, like the iTero, are starting to change the way we are able to approach dental care. Dr. Elizabeth and Dr. Jeff are now able to use these state-of-the-art scanning units to complete your care, helping to make the patient experience smoother and more precise.