By: Dr. Elizabeth Eggert
Vaping, or using e-cigarettes, is smoking a chemical vapor that delivers nicotine into your lungs. Often misconstrued as a safer alternative to traditional cigarettes because there is no tobacco involved, vaping has devastating effects on a person’s oral and overall health. At Eggert Family Dentistry, we think it’s important to educate our patients about the many ways that vaping can affect oral health.
Dangerous ingredients
While vaping liquid doesn’t contain tobacco, it does contain numerous other ingredients that pose a threat to oral health:
Propylene glycol: Used as a carrier ingredient in e-liquid, propylene glycol is a slightly-sweet, colorless liquid that, when vaped, breaks down into acetic acid, lactic acid and propionaldehyde – all of which have toxic effects on soft tissue and enamel.
Nicotine: There are many side effects that can result from nicotine exposure, including reduced blood flow which can cause gum tissue to die. When this happens, gums recede and expose more of the tooth which leads to tooth sensitivity, an increase in cavities and in some cases, tooth loss.
Flavorings: In order to appeal to a wider audience, e-liquid often contains fruit, candy and other flavorings. These flavorings, when added to vegetable glycerin, cause a 27% decrease in the hardness and integrity of tooth enamel.
Oral health complications
Dry mouth: Nicotine in e-liquid inhibits saliva production which leads to dry mouth. When your mouth is dry, it’s a perfect habitat for bacteria which can lead to tooth decay.
Bruxism: Because nicotine is a muscle stimulant, it can cause clenching, gnashing and teeth grinding which, over time, results in wear to enamel and can lead to fractured teeth.
Gum disease: Exposure to nicotine-laden vape liquid can swell and inflame gums. When gums are irritated, your mouth is dry and there are more bacteria on the scene, gum disease easily sets in.
Damage to oral tissue: In rare cases, the lithium batteries in vaping devices overheat and explode, causing extreme damage to oral tissue – damage that can result in permanent disfigurement. There are even a couple documented cases of accidental death related to these explosions.
We want our patients to enjoy optimal dental health! If you have questions or concerns about the effects of vaping on your oral health or the oral health of a loved one, give Dr. Elizabeth Eggert or Dr. Jeff Eggert a call at 651.482.8412. We would be happy to speak with you!



 Sleep apnea
Sleep apnea If a patient comes into our office with jaw pain, Dr. Elizabeth or Dr. Jeff evaluate many things, including the patient’s teeth and jaw. Because sinus problems can be a contributing factor to teeth and jaw discomfort, if their examination is inconclusive, Dr. Elizabeth or Dr. Jeff will refer our patient to an ENT for further evaluation.
If a patient comes into our office with jaw pain, Dr. Elizabeth or Dr. Jeff evaluate many things, including the patient’s teeth and jaw. Because sinus problems can be a contributing factor to teeth and jaw discomfort, if their examination is inconclusive, Dr. Elizabeth or Dr. Jeff will refer our patient to an ENT for further evaluation. Another common cause of jaw pain is a disorder of the temporomandibular joint (TMJ). At Eggert Family Dentistry, we most commonly treat
Another common cause of jaw pain is a disorder of the temporomandibular joint (TMJ). At Eggert Family Dentistry, we most commonly treat 


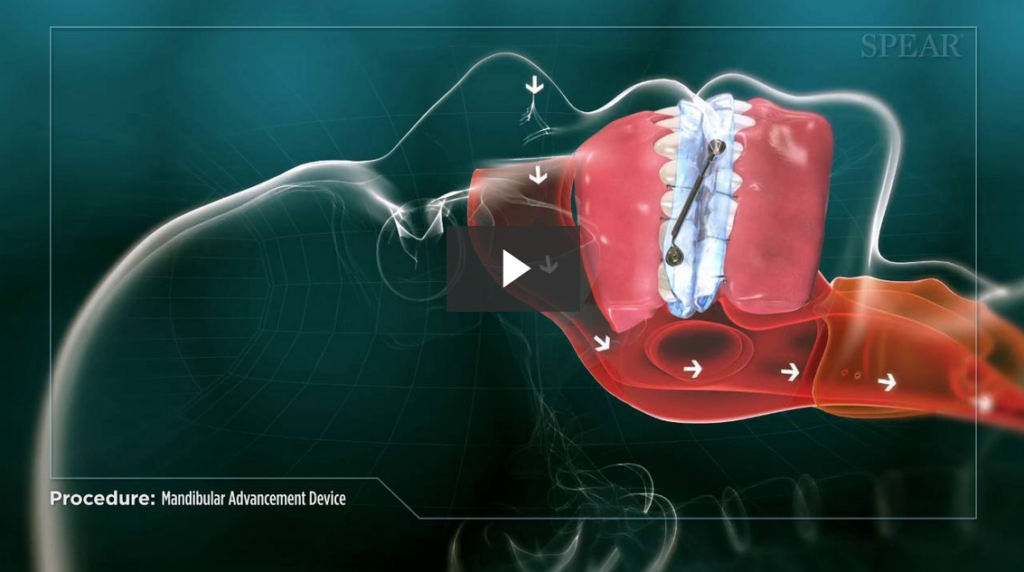
 For some, thinking of sleep apnea conjures up visions of a restless night’s sleep and CPAP machines. While these are certainly the experiences of some patients with this condition, the Seattle Protocol can help many patients with sleep disordered breathing determine if an airway compromise is contributing to their ailments.
For some, thinking of sleep apnea conjures up visions of a restless night’s sleep and CPAP machines. While these are certainly the experiences of some patients with this condition, the Seattle Protocol can help many patients with sleep disordered breathing determine if an airway compromise is contributing to their ailments.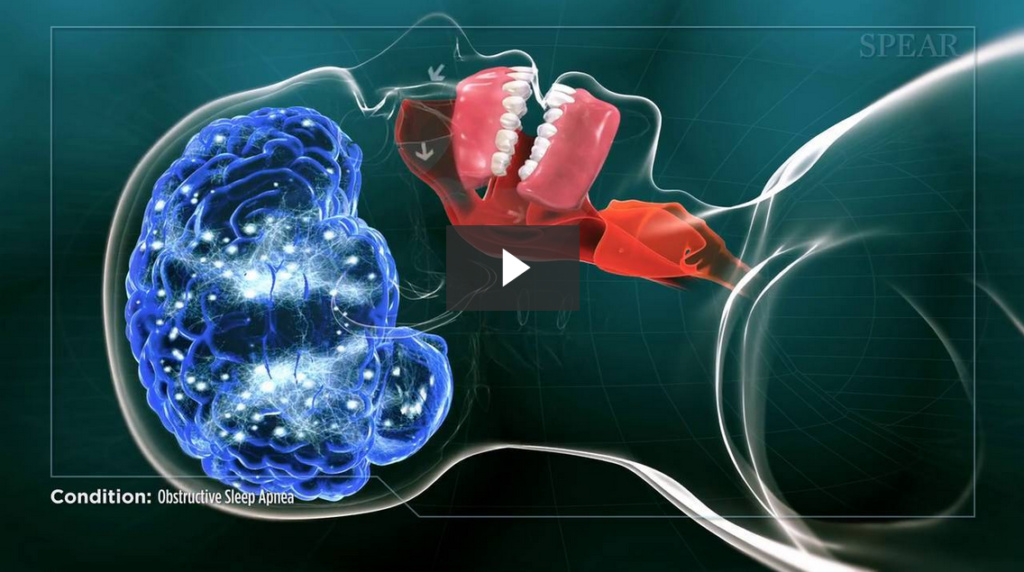

 These conditions may seem unrelated, but new research has found a connection between chronic headaches and sleep apnea and
These conditions may seem unrelated, but new research has found a connection between chronic headaches and sleep apnea and  Once we’ve diagnosed you with TMJ disorder, we’ll discuss your options for treating it. Many patients benefit from an
Once we’ve diagnosed you with TMJ disorder, we’ll discuss your options for treating it. Many patients benefit from an 
 2. You’re taking a medication that may cause tremors as a side effect.
2. You’re taking a medication that may cause tremors as a side effect.
