By: Dr. Elizabeth Eggert
Misaligned teeth can negatively impact a person in several ways. From low self-esteem to problems with teeth and gums and systemic issues, pursuing treatment to realign teeth has many benefits.
One culprit of misaligned teeth is the underbite, dentally referred to as a Class III occlusion. While not as common as its counterpart, the overbite, underbites affect 5-10% of the population.
What causes an underbite?
An underbite occurs when the lower jaw protrudes past the upper teeth when a person’s mouth is in a resting position and can be slight, moderate or severe. With an underbite, teeth don’t line up properly. The bottom front teeth don’t rest behind the top front teeth and the molars don’t stack up neatly.
While this bite is commonly genetic, it can also happen as the result of injury to the jaw, or in childhood from extended use of a pacifier or bottle or from thumbsucking.
An underbite is one of the leading causes of TMD.
If left untreated, what complications can occur?
In addition to low self-esteem, there are a number of physical issues a person with an underbite may deal with:
- Difficulty biting or chewing
- Difficulty forming words properly which can result in lisping or slurred speech
- Difficulty breathing
- Difficulty sleeping
- Sleep apnea
- Cranial discomfort in the form of headaches, jaw pain and/or earaches
- Misaligned teeth
- Bacteria buildup in the mouth which can lead to gingivitis or periodontitis
- Misshapen face
Treatment options for an underbite
If you come into our office with an underbite, Dr. Elizabeth or Dr. Jeff will recommend one of a few courses of treatment:
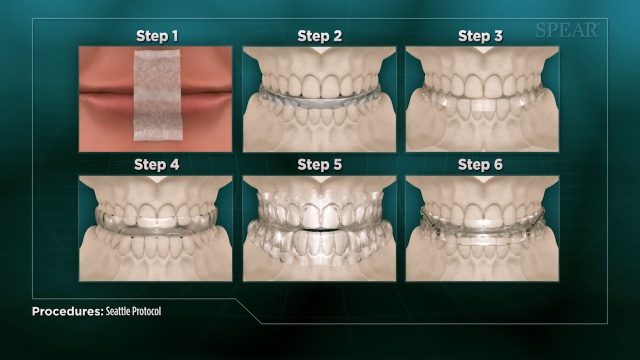
Reverse-pull face mask: A type of headgear, this device helps pull the upper jaw forward by attaching to metal bands on the back of the upper teeth.
Upper jaw expander: Also known as a palatal expander, this device is placed on the roof of the mouth and widened each night. It helps to widen the dental arch and realign the jaws. It’s often used in combination with another common treatment option: braces.
Braces: Braces can contribute to underbite correction by aligning and closing gaps between teeth.
Surgery: In the case of a severe underbite, jaw surgery may be required.
Depending on which treatment option Dr. Elizabeth or Dr. Jeff decide is best to correct your overbite, they may refer you to an orthodontist or oral surgeon and work alongside them to help you achieve your perfect smile.
Is an underbite making you feel self-conscious and leading to other uncomfortable or worrisome issues? Give us a call today at Eggert Family Dentistry to set up a consultation! 651.482.8412.



 While we may tend to villainize sugar, as humans we are biologically predisposed to crave sugary foods and beverages during times in our lives when we need more calories. This is especially true of babies and adolescents whose bodies are growing rapidly. Not only does sugar satisfy a craving and provide the calorie boost growing bodies are looking for, but it has been widely recognized to
While we may tend to villainize sugar, as humans we are biologically predisposed to crave sugary foods and beverages during times in our lives when we need more calories. This is especially true of babies and adolescents whose bodies are growing rapidly. Not only does sugar satisfy a craving and provide the calorie boost growing bodies are looking for, but it has been widely recognized to  When your toddler consumes sugar, it’s often in the form of fruit juice and in some cases, soda. But what actually happens to your child’s teeth when they drink a sugary beverage?
When your toddler consumes sugar, it’s often in the form of fruit juice and in some cases, soda. But what actually happens to your child’s teeth when they drink a sugary beverage?
 When you bring your baby in for their first dental visit, Dr. Elizabeth or Dr. Jeff will take a peek in their mouth and check all erupted teeth to make sure they’re healthy. Then they will discuss basic baby and toddler oral care, address the
When you bring your baby in for their first dental visit, Dr. Elizabeth or Dr. Jeff will take a peek in their mouth and check all erupted teeth to make sure they’re healthy. Then they will discuss basic baby and toddler oral care, address the 
 Buy your child a new toothbrush, a tube of
Buy your child a new toothbrush, a tube of  Check the school’s gum policy and, if it’s allowed, give your child a pack of sugar-free gum to chew after lunch to help clean their teeth
Check the school’s gum policy and, if it’s allowed, give your child a pack of sugar-free gum to chew after lunch to help clean their teeth Crunchy foods like carrots, celery and apples; limit citrus fruits which erode enamel quickly
Crunchy foods like carrots, celery and apples; limit citrus fruits which erode enamel quickly Put a travel toothbrush, a small tube of fluoride toothpaste, a container of floss and a container of dental wax in a small zipper bag and encourage them to brush their teeth after lunch
Put a travel toothbrush, a small tube of fluoride toothpaste, a container of floss and a container of dental wax in a small zipper bag and encourage them to brush their teeth after lunch



 The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck.
The first time we see you for sleep apnea symptoms, we will perform an assessment for signs of structural abnormalities or any physical issues that could be contributing to airway obstruction. This could include an enlarged tongue or tonsils, a small jaw or a large neck. A
A 
 When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others:
When you come in for an appointment, we look for signs or symptoms that could be considered “red flags” for airway conditions, including sleep apnea. Dr. Elizabeth or Dr. Jeff perform an assessment to see if you have any of the following risk factors among many others: Did you know that, in
Did you know that, in  Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
Bruxism is another condition that is often present alongside obstructive sleep apnea. Often intertwined with TMD, bruxism describes a condition caused by the clenching or grinding of teeth. It occurs unconsciously during sleep and can be another way a person’s body compensates for an airway obstruction.
